Given the special situation, including the epidemiological context in Ukraine and the existence of an increased influx of people in Romania who can be accommodated in other locations than organized (refugee camps, immigration centers, accommodation established by county committees for situations We warn that there is a risk of communicable diseases, including measles.
The risk is increased for the following reasons:
– the existence of vaccines against measles at national level below 95% – the effective control of this disease requires a constant vaccination coverage of over 95%,
– measles epidemics in Ukraine due to suboptimal vaccine coverage,
– increase in the number of refugees from Ukraine in the near future.
There have already been reported 2 confirmed cases of measles in the local population (1 case in Bacău County and 1 case in Satu Mare County). On 16.03.2022, another 3 suspected cases of measles were reported under investigation (1 case in Suceava County for a refugee child from Ukraine and 2 cases in Satu Mare County – children belonging to the local population).
The only way to protect against measles is to get vaccinated.
It is necessary to continue the activity of measles vaccination of the local population and to inform
belonging to refugee children regarding the possibility of routine vaccination in Romania.
The MMR vaccine
The MMR (measles, mumps and rubella) vaccine is a combined vaccine that protects against measles, mumps and rubella. The MMR vaccine is safe and effective and has very few side effects. Mild reactions have been reported, such as fever, redness and swelling at the injection site. Some vaccinated people get a mild non-infectious rash on their skin, similar to the one that occurs in the case of measles, usually after 7-14 days after vaccination, which disappears within 1-3 days.
Two doses of vaccine are needed for maximum protection. The first dose of MMR vaccine should be given at 12 months of age and offers: 95% protection against measles, 80% protection against mumps, 90% protection against long-term rubella. The second dose of MMR vaccine should be given at the age of 5 and offers: 99.7% protection against measles, but up to 5% of immunized people may lose their protection over time, 80-95% protection against mumps.
The MMR vaccine can also be given at a younger age if there are outbreaks. Infants between the ages of six and nine months in an area – or about to travel to areas – at high risk for measles exposure should receive an additional dose of MMR vaccine. The dose given before the age of nine months is an additional dose to the two doses included in the national vaccination program, intended to ensure complete protection.
If possible, within 3 days of contact with a person suffering from measles, mumps or rubella, unvaccinated persons from the age of 9 months or persons who have not been vaccinated or have been vaccinated only once or are unclear immunization status, you should receive an MMR vaccine.
Who should not be vaccinated?
People suffering from an acute illness with a fever higher than 38.5 ° C will be vaccinated only after recovery. People with immunodeficiency – congenital, acquired, drug-induced – generally cannot be vaccinated. Exceptions are possible in certain circumstances. These patients should seek medical advice to find out if they can receive the MMR vaccine with that immunodeficiency and after assessing the risks and benefits. Consult your doctor if symptoms of the disease have occurred after a previous MMR vaccination or if there is severe hypersensitivity to the vaccine components. People with a severe egg protein allergy (anaphylactic reaction after eating egg whites) can generally be vaccinated, but vaccination should be done with the necessary precautions.
MMR vaccination should not be given to people who have received immunoglobulin in the last few months (3 to 8 months, depending on the dose of immunoglobulin used) or who have had blood transfusions during the same period (due to protective substances – antibodies – in the donated blood, the vaccine may remain ineffective against the viruses mentioned). MMR vaccination should not be given to pregnant women, as there is a theoretical risk to the fetus due to vaccine viruses. For the same reason, a possible pregnancy should be prevented for a period of 1 month after vaccination. However, accidental vaccination during pregnancy is not considered a reason for abortion.
Possible local and general side effects after vaccination
After MMR vaccination, at approx. 10% of those vaccinated may experience pain, swelling and redness at the injection site. This is a normal manifestation of the body’s confrontation with the vaccine and occurs within 1 to 3 days after vaccination, rarely lasts longer.
Occasionally (between 0.1 and 1%) the nearby lymph nodes swell.
Common symptoms such as headaches, fatigue, general discomfort, or gastrointestinal disorders can occur frequently (between 1 and 10%).
Frequently, usually 5 to 12 days after vaccination, mild symptoms of a non-contagious measles, mumps or rubella infection, the so-called vaccine disease, may develop.
Between 5 and 15% of those vaccinated have a fever, often (about 2%) also associated with a measles-like rash.
Temporary joint discomfort has been observed in adolescents and adults, which is very rare in children.
Are complications possible after vaccination?
Complications following vaccination are those consequences that go beyond the reactions considered normal after vaccination and that significantly affect the health of the vaccinated person. If an infant or young child reacts to the MMR vaccination with fever, febrile seizures may rarely occur. This usually goes without saying.
Allergic reactions are very rare. These are generally due to vaccine excipients, such as gelatin or antibiotics (contained in traces). Anaphylactic shock has been reported only in isolated cases.
Also, in isolated cases, bruising was achieved after vaccination due to the reduction in platelet counts. Usually, they disappear quickly and without consequences, more severe evolutions existing only in isolated cases.3
Prolonged inflammation of the joints has been observed in adolescents and adults.
There is no indication that the attenuated urlian virus used in this vaccine may cause meningitis.
Other diseases of the nervous system (eg convulsions, discomfort, temporary paralysis) or vascular inflammation in correlation with the time of vaccination have been reported very rarely in the medical literature.
Note: An allergy to egg proteins is not a contraindication to MMR vaccination, as measles and mumps vaccine viruses are not grown on chicken eggs, but on embryonic chicken cells.
Vaccine safety
In 40 years, more than 500 million doses of MMR have been administered in about 100 countries.
Its safety has been closely monitored in many countries, e.g. in Finland, where children have received two doses of MMR since 1982. The reactions reported after MMR were followed for a period of 14 years. MMR has proven to be a very effective vaccine, with great results in terms of safety.
There is no evidence of a link between MMR (MMR) and autism or inflammatory bowel disease.. Extensive research has been conducted in the UK and many other countries on the possible link between the MMR vaccine (MMR) and autism, in which hundreds of thousands of children have participated. No connection found.
Vaccine coverage
Vaccine coverage with MMR in Neamț County:
– for children aged 18 months, born in July 2019 – 79.21%
– in the cohort of newborns from 2015 – 68.38%
– for 12-month-old children born in July 2020 – 72.87%
– for 24-month-old children, born in July 2019 – 84.49%
What is measles?
Measles is a highly contagious viral disease that can be contracted at any age and can be
spread widely.
symptom
Measles symptoms usually appear 10-12 days after infection:
• the initial symptoms are similar to those of a cold with rhinorrhea, cough and mild fever;
• eyes turn red and become sensitive to light;
• between days 3 and 7, the temperature can reach up to 41 ⁰C;
• red rash that lasts between 4 and 7 days first appears on the face and then spreads all over the body;
• Small white spots may also appear on the gums and inside the cheeks.
What are the complications of measles?
Complications, such as otitis and diarrhea, can occur in 30% of children and adults with measles.
Pneumonia is a potentially serious complication that can lead to the death of some patients with measles. Pneumonia is the leading cause of death among measles-related deaths.
The measles mortality rate is 1-3 people per 1,000 cases, with the highest risk in children under five and immunocompromised people.4
Inflammation of the brain tissue (encephalitis) occurs in about 1 in 1,000 patients with measles, a condition that leads to permanent neurological impairment in about one in four cases.
Very rarely, a persistent measles virus infection can cause subacute sclerosing panencephalitis (PESS), a disease in which nerves and brain tissue progressively degenerate and are more likely to occur if the measles infection occurs at an early age. PESS usually occurs a few years after the measles patient becomes ill, on average 7-10 years after infection. Symptoms include personality changes, gradual deterioration of mental state, muscle spasms and other neuromuscular symptoms. PESS does not heal and always leads to death.
How is measles transmitted?
The measles virus is transmitted by airborne splashes when the infected person coughs or sneezes. Sprays containing the virus can remain in the air for several hours, and on contaminated surfaces the virus remains contagious for up to 2 hours. The sick person can transmit measles just before the rash (usually 4 days) and for about 4 days after the rash.
Measles is easily spread among unvaccinated people. It is estimated that a person with measles can transmit the infection to an average of 12-18 unprotected people.
How is measles treated?
There is no specific treatment for measles. Most people recover from supportive care, which may include hydration and fever medications.
Antibiotics are not effective against measles because the disease is caused by a virus. However, antibiotics are often used to treat complications with bacterial infections that can occur due to measles, such as pneumonia and otitis.
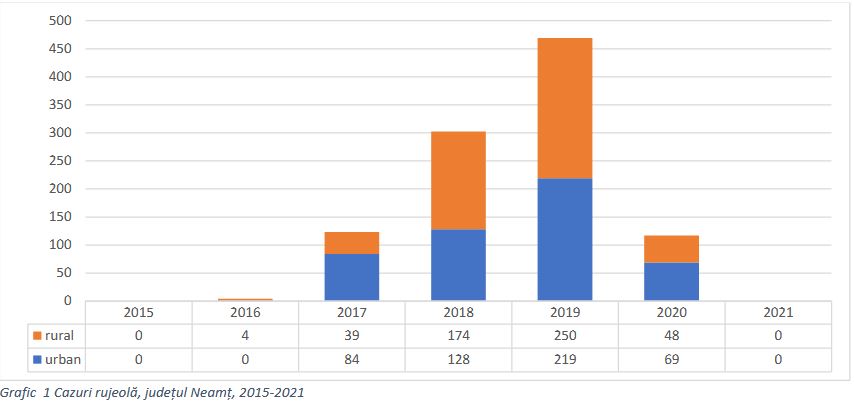
Measles cases in Neamț county
In Romania, from the beginning of the measles epidemic (2016) to its end (2020), there were 20,204 cases of measles, resulting in 64 deaths.
–