Vienna, Austria – According to the proof U-ACHIEVE Maintenance in ulcerative colitis (UC) presented in the opening session of the 30th European Gastroenterology Week (UEGW, 8-11 October 2022, Vienna, Austria)[1]the anti-JAK upadacitinib, whose efficacy had already been demonstrated in induction treatment, is also effective in maintenance treatment.
Upadacitinib is a selective and reversible oral inhibitor of Janus kinase (JAK 1 and JAK 1/3). Janus kinases (for Just Another Kinase; JAK) form a family of intracellular tyrosine kinases, without receptor function. These molecules allow the transduction of cytokine source signals through the JAK-STAT pathway (Janus kinase-signal transducer and activator of the transcription pathway) and are involved in a wide range of cellular processes, including inflammatory responses, hematopoiesis and immune monitoring.
The superior efficacy of upadacitinib to placebo was already demonstrated in moderate to severe active ulcerative colitis (UC) in two previously published phase 3 induction studies: U-REACH induction[2] et U-COMPLETE[3].
Patients with a clinical response according to the Mayo UC-DAI score adapted, with upadacitinib 45 mg / day after eight weeks of induction treatment, were then included in the U-ACHIEVE maintenance program. Data on the efficacy of U-ACHIEVE Maintenance in 52 weeks were presented at this edition of UEGW; they are positive.
Differences in efficacy from the placebo arm are the largest observed in IBD with anti-TNF-α infliximab.
Upadacitinib effective on clinical remission rate at 52 weeks
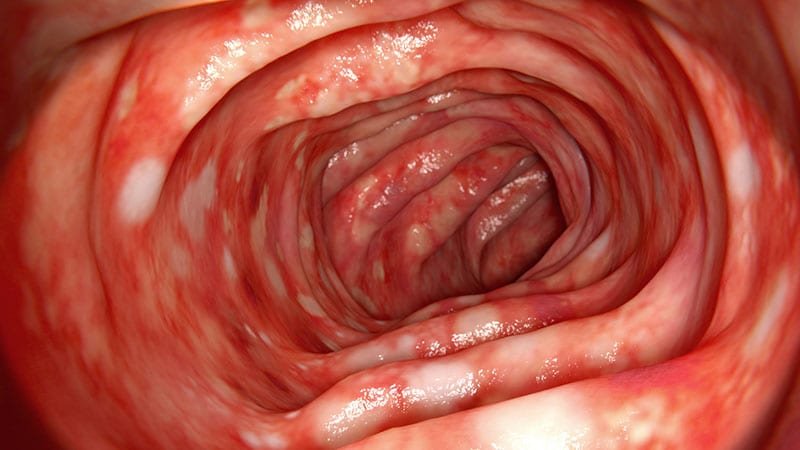
According to the U-ACHIEVE maintenance protocol, 651 patients with moderate to severe UC who responded to induction therapy with upadacitinib (UPA) 45 mg / day at week eight were randomized into three treatment groups and followed for 52 weeks: placebo, upadacitinib 15 mg / day and upadacitinib 30 mg / day. The primary objective of the study was the clinical remission rate as defined by a modified Mayo score of less than or equal to 2 (stool frequency score ≤ 1, rectal bleeding = 0, endoscopic secondary score ≤ 1).
The primary endpoint of the study was met with the two maintenance doses of upadacitinib and with all secondary endpoints including clinical response, sustained clinical remission with or without corticosteroids, sustained clinical response, endoscopic improvement defined by a secondary endoscopic score ≤ 1, endoscopic remission defined by an endoscopic sub-score of 0, as well as histological response and remission defined by a Geboes histological score of less than 3.1 or 2.
A higher proportion of patients achieved the primary endpoint of clinical remission at week 52 with upadacitinib 15 mg / day (40.4%) and upadacitinib 30 mg / day (53.6%) compared to placebo (10.8%) ; both p <0.001), since as well as all secondary endpoints, such as endoscopic improvement and remission, maintenance of clinical remission, clinical remission without corticosteroids, and histological-endoscopic improvement of the mucosa.
Acceptable long-term tolerance
In terms of safety, no new signals have been described, with more asymptomatic increases in creatine kinase and more herpes infections in patients taking upadacitinib. Overall, 746 patients were evaluated for safety (UPA 15 mg / day, n = 250; UPA 30 mg / day, n = 251; placebo, n = 245). Of these, 8.4% experienced a serious adverse event (AE) with UPA15, 8.4% with UPA30 and 9.4% with placebo; 4%, 7.2% and 10.2% experienced adverse events leading to treatment discontinuation, respectively.
The most common adverse events included worsening of UC with upadacitinib 15 mg / day (11.6%) and placebo (30.2%) and nasopharyngitis with upadacitinib 30 mg / day (10.4%). No deaths were observed.
Serious infections were reported in 3.6% of patients with upadacitinib 15 mg / day, 2.8% with upadacitinib 30 mg / day and 3.3% with placebo. Herpes zoster has only been reported with upadacitinib (UPA 15 mg / day: 4.8%; UPA mg / day 30: 5.6%). Malignant tumors excluding non-melanoma skin cancer were reported by one patient with PBO, another with UPA 15 mg / day and two with UP A 30 mg / day.
Major adverse cardiovascular events were reported in one patient each receiving placebo and UPA 30 mg / day, while venous thromboembolic events were reported in two patients each on UPA 15 mg / day and UPA 30 mg / day, none on placebo.
Both doses of upadacitinib were well tolerated with no new signals.
“In ulcerative colitis patients who responded to induction treatment, UPA 15 mg / day and UPA 30 mg / day were significantly more effective than placebo as maintenance therapy for all primary and secondary endpoint assessments,” concluded the Severine Vermeire (department of hepato-gastroenterology, University Hospital of Leuven, Belgium) who presented the study in plenary session. Both doses of upadacitinib were well tolerated with no new signs in a larger patient population than previously reported. These results are consistent with previously published data. “
“This study reinforces the fact that anti-JAK upadacitinib is not only effective in induction treatment but also in the maintenance of UC,” commented the Mr. David Laharie (department of hepato-gastroenterology, University Hospital of Bordeaux) for Medscape French edition, as in Crohn’s disease. Furthermore, the efficacy of this anti-JAK is undoubtedly high because the differences in efficacy compared to the placebo arm are the greatest observed in IBD from the anti-JAK.TNF-α infliximab ”
Vedolizumab, more effective in recent Crohn’s disease
Vedolizumab (monoclonal antibody against integrin α4β7) is prescribed for the induction and maintenance treatment of Crohn’s disease (CD). But while anti-TNFs are known to be all the more effective as the disease is recent, this remains to be demonstrated for this immunomodulator. I study LOVE-CD2 (Belgium, Netherlands, Hungary) 4, also presented at the congress, has just shown it: this open-label prospective multicenter study, at least the 6-month interim analysis on a small number, found greater efficacy of vedolizumab in early CD (duration of evolution less than 2 years, and having benefited only from corticosteroid and / or immunomodulatory treatments), compared to the main criterion of combined steroid-free clinical and endoscopic remission. A caveat, however, specifies David Laharie: “Crohn’s disease patients qualified as ‘late’ have been exposed to anti-TNFs, which in themselves likely modify the response profile to vedolizumab. Furthermore, the duration of evolution of Crohn’s disease was also highly variable in this subgroup, ranging from 3 to 41 years. ”
Links of interest:
Le Pr Severine Vermeire a reçu des subventions de la parte: AbbVie, J&J, Pfizer and Takeda; and has received consulting and / or conference fees from AbbVie, Arena Pharmaceuticals, Avaxia, Boehringer Ingelheim, Celgene, Dr. Falk Pharma, Ferring, Galapagos, Genentech-Roche, Gilead, Hospira, Janssen, Mundipharma, MSD, Pfizer, Prodigest, Progenity, Prometheus, Robarts Clinical Trials, Second Genome, Shire, Takeda, Theravance and Tillots Pharma AG.
The Pr David Laharie declares links of interest with the Abbvie, BMS, Celltrion, Ferring, Galapagos, Janssen, Lilly, MSD, Novartis, Pfizer, Prometheus, Roche, Takeda laboratories.
Follow Medscape in French on Twitter.
Follow theheart.org | Medscape Active Cardiology Twitter.
Sign up for the Medscape newsletter: select your choices