– Why doctor: Like every year, the communication operation called “Mars Bleu” raises awareness for a month in France about colorectal cancer. What are the right things to do on a daily basis to avoid developing it?
Dr Raphaël Bourdariat – There is no absolute prevention of the appearance of colorectal cancer, but we can nevertheless reduce the probability of seeing it appear. For this, a healthy lifestyle will greatly help to limit the risks. We think in particular of tobacco, a factor that promotes carcinogenesis (the production of cancer). Regular practice of sport, as well as the fight against a sedentary lifestyle and being overweight, will also reduce the risk of the onset of the disease. Adopting a healthy diet is also essential.
– Are there any foods to avoid or favor?
There are no foods to completely banish, but choosing a varied and balanced diet will help considerably to prevent the appearance of the pathology. Nutritional factors that increase the risk of colorectal cancer are: diets high in protein, especially red meat, and diets too high in fats, especially those of animal origin.
Other nutritional factors are, on the other hand, rather protective: coffee, dietary fiber (mainly contained in vegetables such as cabbage) and vitamins A, C, D or E. Aspirin and anti-inflammatory drugs can also be considered as preventive elements.
– What about screening?
Always with a view to prevention, it will be necessary to detect people at risk in relation to their family history and to set up close monitoring with them if necessary by colonoscopy.
For the general French population, the public health authorities have generalized a test allowing the search for blood in the stool from the age of 50. It must be renewed every two years and aims to identify early people who could potentially develop early colon or rectal cancer.
– How does colorectal cancer develop?
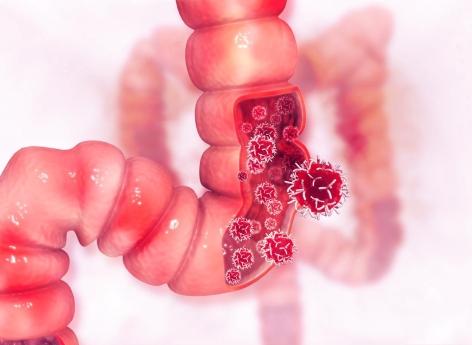
The colon (or large intestine) is the terminal part of the digestive tract. It follows the small intestine (or small intestine) and ends with the rectum. The function of the large intestine is essentially to reabsorb as much liquid as possible from food in order to concentrate, form and store faeces, residues of digestion.
The common point between the colon and the rectum is the intestinal mucosa, the wall lining the inside of the intestine and formed of villi covered with superficial cells (the epithelium). This mucosa can, under the influence of mutations, gradually turn into cancerous tissue.
First, there are so-called “adenomatous” polyps, which are benign tumours. Then, in a second step, it comes to cancers called “Lieberkühnian adenocarcinomas”. The cancerous (malignant) cells then proliferate unchecked. The tumor first develops in the wall of the intestine, then the cancerous cells migrate to the lymph nodes and, later, throughout the body, possibly giving rise to metastases.
– Is colorectal cancer common?
Colon and rectal cancers are among the most frequent cancers in France: in 2009, more than 37,000 new cases were diagnosed.
Statistically, France is one of the countries where this cancer is the most widespread. It is the second cancer in men after that of the prostate (just over 60,000 cases per year), and the second in women after that of the breast (about 42,000 cases per year).
– Are we still dying?
Yes. But its mortality has been decreasing since the 1980s thanks to advances in treatment and diagnosis in the early stages of the disease.
– What are the symptoms of colorectal cancer?
It is from the age of 50 that the risk of seeing this cancer appear increases. Very often, the symptoms appear when the tumor has already reached a certain size.
The most common warning signs are bleeding (not always visible in the stool), anemia (which can manifest as fatigue, shortness of breath and pallor), transit disorders (sudden constipation or long diarrhea) , and colicky pains occurring in crises of a few days.
More rarely, it is a digestive occlusion due to the tumor causing a narrowing of the inside diameter of the colon which leads to making the diagnosis in an emergency. The obstruction causes abdominal pain, gas and vomiting.
Last clarification: for people with hemorrhoids, the risk is to confuse bleeding due to colorectal cancer with bleeding from hemorrhoids. Any abnormal bleeding should therefore lead to consultation with a doctor.
– What are the main risk factors?
Although colon cancer mainly affects people aged around 70, certain risk factors expose people to cancer before this age.
For example, it has been shown that the risk of colorectal cancer increases in the family of a patient with this pathology. It is even more important when two first-degree relatives are affected (parents, brothers or sisters), and especially when the disease occurred before the age of 60.
Likewise, the risk increases with the presence of adenomatous polyps, which have a risk of malignant transformation. The danger is proportional to their size: low below one centimeter and around 30% beyond two centimeters. When they are not too big, the removal of polyps is feasible in the majority of cases during colonoscopy.
Finally, inflammatory diseases of the digestive tract such as Crohn’s disease and ulcerative colitis also increase the risk of cancerous transformation of the cells of the intestine. This danger is all the more threatening if these diseases have been evolving for more than 10 years.
– Is this disease hereditary?
In the vast majority of cases, colorectal cancer is not hereditary. However, nearly 5% of these cancers result from a genetic predisposition, ie their occurrence is linked to the existence of an abnormal gene.
– What treatments are available today?
Surgery is currently the only treatment that can cure colon or rectal cancer. It should therefore be carried out whenever possible.
In the absence of medico-surgical management, the tumor inevitably risks becoming complicated in the long term by haemorrhage, intestinal obstruction or intestinal perforation. These complications will then require emergency surgery and generally require the creation of an artificial anus, which could have been avoided if the operation had been carried out “cold”.
Several types of treatments can be combined with surgery, such as radiotherapy and chemotherapy. In all cases, they are adapted to the characteristics of the tumor and its stage of evolution.
– What does the surgery involve?
The surgery has two objectives: to remove the tumor completely on the one hand, and to specify the stage of evolution of the cancer on the other hand. The type of intervention differs depending on whether it is rectal or colon cancer.
The procedure for colon cancer involves removing the segment of intestine on which the tumor is located. The fat surrounding the colon, in which the tumor could have spread and which contains nodes likely to be invaded, must also be removed. After removal, the two remaining segments of intestine are sutured together to restore digestive continuity. If the tumor is located on the right colon, the surgeon removes the right part of the colon, then performs an ileocolonic anastomosis (that is to say a suture between the ileum – terminal part of the intestine hail – and the remaining colon). If the tumor is located on the left colon or the left part of the transverse colon, the surgeon performs a left colectomy then performs a colonic anastomosis (that is to say a suture between the remaining transverse colon and the sigmoid colon) .
The intervention for rectal cancer varies according to the tumor location. When the attack is located on the upper part of the rectum, the intervention is comparable to that of cancer of the left colon. When it is lower, the operation consists of removing the entire rectum, as well as the fatty and vascular area that surrounds it, called the “mesorectum”. A restoration of the continuity of the digestive tract between the colon and the anus is possible if the lower pole of the tumor is more than one centimeter from the anal sphincter (muscle allowing to control the evacuation of the stools).
– Have there been any innovations in this area?
If the reference technique is, for the moment, conventional surgery, which allows a direct approach to the tumour, laparoscopic surgery is one of the most significant innovations of the last ten years. Its advantage is to reduce the size of the scar, to reduce postoperative pain and the duration of hospitalization. It is done under general anesthesia.
– How is the therapeutic decision made?
The management of colon and rectal cancer requires the intervention of several doctors. In general, the general practitioner is the first to be consulted when symptoms appear. The second speaker is the gastroenterologist performing the colonoscopy to make the diagnosis. Then the radiologist, the pathologist and the biologist carry out the examinations of the extension assessment. Then it is the surgeon who intervenes. Finally, there are oncologists, either for radiotherapy (radiotherapist) or for chemotherapy (oncologist or gastroenterologist specializing in digestive oncology). Care also presupposes the intervention of many other actors (nurses, nursing auxiliaries, psychologists, dieticians, etc.).
Treatments for a patient with colorectal cancer are codified and discussed at medical meetings called Multidisciplinary Consultation Meetings (RCP) which bring together a large number of specialists.
– How do you learn that you have colorectal cancer?
Whenever possible, the patient should benefit from an announcement consultation during which his treatments are detailed.
During this appointment, he can meet a nurse to explain his care and in particular his chemotherapy. He can also then consult a psychologist, likely to help him overcome this difficult period, a dietician, to choose the right diet, and finally a social worker, to guide him in his administrative procedures with work or health insurance.
–