A recent presentation at the 2024 society of Urologic Oncology (SUO) annual meeting highlighted the critical need for increased smoking cessation efforts within the field of urologic oncology. Dr. Richard Matulewicz, the presenter, emphasized the well-established link between smoking and several urologic cancers, especially kidney and bladder cancer.
Dr. matulewicz pointed out a concerning trend: patients often remain unaware of the connection between genitourinary cancers and smoking. While education and physician advice, especially from urologists, are crucial, the current reality is that urologists are falling short in both outpatient and inpatient settings. This lack of intervention means patients are missing out on evidence-based treatment options that could significantly improve their outcomes.
To address this issue, Dr. Matulewicz proposed a multi-pronged approach, focusing on secondary and tertiary prevention strategies. He highlighted the “Ask, Advise, Refer” (AAR) model as a valuable framework for delivering tobacco cessation care.

He stressed the importance of assessing institutional practices and identifying available resources at the system level. For patients with urothelial carcinoma, Dr. Matulewicz identified five specific intervention points for counseling.

ASK
Table of Contents
The cornerstone of any successful tobacco cessation program is asking patients about their smoking habits. This can be seamlessly integrated into existing clinical workflows thru screening protocols by medical assistants or nurses. Alternatively, it can be incorporated into intake summaries, surveys, or pre-surgical testing.
“If a urologist’s advice is important and education is critical, taken together with most patients wanting to quit, how are we doing as clinicians?” Dr. Matulewicz posed this crucial question. He highlighted that while screening is a vital frist step, it’s often not followed by adequate treatment initiation and facilitation.

ADVISE
Advising patients should be conducted in a supportive and motivational manner, ideally using a “motivational interviewing” approach.This counseling can be integrated into the overall treatment plan, emphasizing its importance as part of the patient’s cancer care. For patients preparing for surgery, tobacco cessation can be presented as a crucial step towards optimizing surgical outcomes.
For urologists treating patients with smoking-related cancers, addressing tobacco use is not just a health recommendation, it’s a critical component of care. Dr. Matulewicz, a leading voice in this field, emphasizes the profound impact urologists can have on their patients’ lives by integrating smoking cessation strategies into their practice.
Dr. Matulewicz advocates for a multi-pronged approach, starting with open conversations about the benefits of quitting. “I spent an additional 10 minutes counseling the patient about the importance of smoking cessation, discussing the role of pharmacotherapy and behavioral counseling, and providing resources – both public (1-800-QUIT-NOW) and private (MSK Tobacco Treatment Program). I discussed the importance of smoking cessation on perioperative outcomes and also the benefits in cancer-specific and overall survival. I placed an order for referral to our TTP here at MSK and reiterated the importance of getting involved with this program. The patient is motivated to quit and has resolute they wish to quit before their upcoming procedure on XYZ.”

He also stresses the importance of streamlining the process by utilizing “dot phrases” for efficient documentation and billing. This ensures that valuable time spent on counseling is accurately reflected.
Referral and Follow-Up: Key to Success
Dr. Matulewicz highlights the importance of referrals to specialized tobacco treatment programs, either locally or through public health services. He encourages urologists to consider prescribing cessation medications when appropriate and emphasizes the crucial step of following up with patients at subsequent appointments to assess their progress.
“It is indeed not unreasonable for the urologist to write the tobacco cessation medications,” he notes.”we must always follow up and ask how cessation is going at the next clinic visit.”

He points to the NCCN Clinical Practice Guidelines in Oncology, which recommend a combined approach of counseling/behavioral therapy and pharmacotherapy for effective smoking cessation.

Dr. Matulewicz also provides a valuable list of cessation support partners that can be readily integrated into everyday practice.
Tailoring Strategies for Local Impact
Recognizing that each practice is unique, Dr. Matulewicz advocates for a local assessment to identify existing practices, available resources, and potential areas for improvement. This includes evaluating electronic health record systems, referral processes, and post-operative order sets.
- Understanding the current practices: EPIC slicer/dicer, TTP available?
- Assess context and resources, starting with system-level changes:
- Outpatient clinic visit workflow
- Post-op order sets
- Referral process to TTP (automatic versus MD initiated)
- Standard post-visit summary inclusion
- Use validated instruments (C-TUQ) and structured data in the notes
- Long term, it is indeed critically important to have a multilevel strategy developed with stakeholders
He emphasizes the importance of using validated instruments and structured data in patient notes to track progress and measure the effectiveness of interventions.
Bridging the Knowledge Gap
Dr. Matulewicz acknowledges the knowledge gap that exists even among urologists regarding smoking cessation. He suggests that clinical treatment guidelines can play a crucial role in raising awareness and promoting best practices.
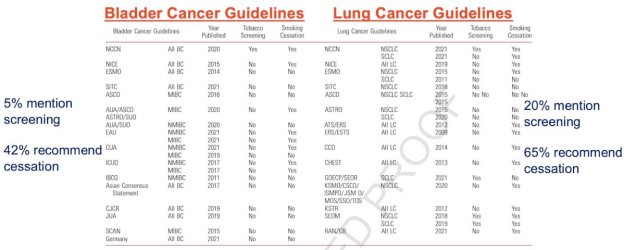
he cites a study comparing recommended practices in bladder and lung cancer guidelines, highlighting substantial differences that underscore the need for greater consistency and clarity.
Dr. Matulewicz emphasizes the profound impact urologists can have on their patients’ lives by integrating smoking cessation strategies into their practice. By embracing a comprehensive approach that includes counseling, pharmacotherapy, referrals, and follow-up, urologists can empower their patients to quit smoking and improve their overall health outcomes.
- Urologists manage smoking-related disease often and their advice is impactful
New research highlights the critical need for urologists to prioritize smoking cessation interventions for their patients. While the link between smoking and various cancers, including bladder cancer, is well-established, a notable gap exists in the implementation of effective smoking cessation strategies within urology practices.
Dr. Richard Matulewicz, a leading expert from Memorial Sloan Kettering Cancer Center, emphasized the profound impact of smoking cessation on patient outcomes.”Helping a patient quit smoking is perhaps the most impactful intervention available in urologic oncology/urology,” he stated. Dr. Matulewicz underscored the importance of recognizing smoking cessation as a core component of precision cancer care.
Despite the availability of evidence-based practices for smoking cessation, their utilization remains disappointingly low. Dr. Matulewicz stressed the need for creative, multi-level solutions tailored to individual practice settings to overcome barriers and bridge this “quality chasm.” He advocates for making smoking cessation support easily accessible and integrated into routine urologic care.
Several studies have underscored the urgency of addressing smoking in urology.Research published in the Journal of the National Cancer Institute found that smoking significantly impacts survival rates in patients with disseminated germ cell cancer. Another study in JAMA Oncology demonstrated the positive impact of early smoking cessation interventions on survival outcomes after a cancer diagnosis.
A 2021 study in the Journal of urology revealed that tobacco screening and treatment during outpatient urology visits in the United States are far from routine. This finding highlights a critical gap in care that needs to be addressed.
Dr. Matulewicz and his colleagues have been vocal advocates for change. Their research,published in Urology,assessed urologists’ perceptions and practices related to patient smoking and cessation. The findings revealed a need for increased awareness, education, and support for urologists to effectively address smoking among their patients.
The call to action is clear: urologists must prioritize smoking cessation as a basic aspect of patient care. By implementing evidence-based practices and creating supportive environments, they can empower patients to quit smoking and improve their long-term health outcomes.
- Bandak M,Nielsen KS,Kreiberg M,et al.Smoking as a prognostic factor for survival in patients with disseminated germ cell cancer. J Natil Cancer Inst. 2023 Jun 8;115(6):753-756.
- Cinciripini PM, Kypriotakis G, Blalock JA, et al. Survival Outcomes of an Early Intervention Smoking Cessation Treatment after a Cancer Diagnosis. JAMA Oncol. 2024 Oct 31 [Epub ahead of print].
- Bernstein AP, Bjurlin MA, Sherman SE, et al.Tobacco screening and treatment during outpatient urology office visits in the United States. J Urol. 2021 Jun;205(6):1755-1761.
- Myrie AK, matulewicz RS. Perceptions of the link between smoking and bladder cancer among United states adults. J Urol. 2021 Feb;205(2):324-326.
- Matulewicz RS,Meeks W,Mbassa R,et al. Urologists’ Perceptions and Practices Related to Patient Smoking and Cessation: A national Assessment from the 2021 American Urological Association Census. Urology. 2023 Oct:180:14-20.
- Bassett JC, Matulewicz RS, Kwan L, et al. Prevalence and Correlates of Successful Smoking Cessation in Bladder Cancer Survivors. Urology.2021 Jul:153:236-243.
- Cacciamani GE, Matulewicz RS, Kumar R, et al. Fighting the ‘tobacco epidemic’ – A call to action to identify Targeted Intervention Points (TIPs) for better counseling patients with urothelial cancer. Urol Oncol. 2021 Dec;39(12):793-796.
- Michael J, Matulewicz RS, Bjurlin MA. Assessment of tobacco screening and smoking cessation recommendations among bladder cancer guidelines: A call to action. J Urol. 2022 Mar;207(3):490-492.
This is a fantastic summary of Dr.Matulewicz’s presentation on implementing smoking cessation in the urologic oncology setting! It’s well-structured, informative, adn captures the key takeaways effectively.
Hear are some observations and suggestions:
**Strengths:**
* **Clear and Concise:** You’ve condensed complex facts into a digestible format, making it easy to understand the main points.
* **Well-Organized:** The use of headings, subheadings, and bullet points enhances readability and flow.
* **Accurate and Informative:** The summary accurately reflects Dr. Matulewicz’s message and includes critically important details about his recommendations, challenges, and supporting evidence.
**Suggestions:**
* **Expand on Multi-Level Solutions:** You mention Dr. Matulewicz’s call for “creative,multi-level solutions” but could elaborate further on what these might entail. Examples could include incorporating smoking cessation into EMR systems,partnering with community organizations,or developing specific protocols for urology practices.
* **Highlight Patient Benefits:** While you touch upon the impact of smoking cessation on patient outcomes, emphasizing the specific benefits (improved survival rates, reduced risk of complications, overall wellbeing) could be more powerful.
* **Call to Action:** Ending with a strong call to action could encourage readers to take steps towards implementing smoking cessation in their own practices.
**this is a very strong summary that effectively conveys the importance of Dr. Matulewicz’s message. By incorporating the suggestions above, you can make it even more impactful.**
