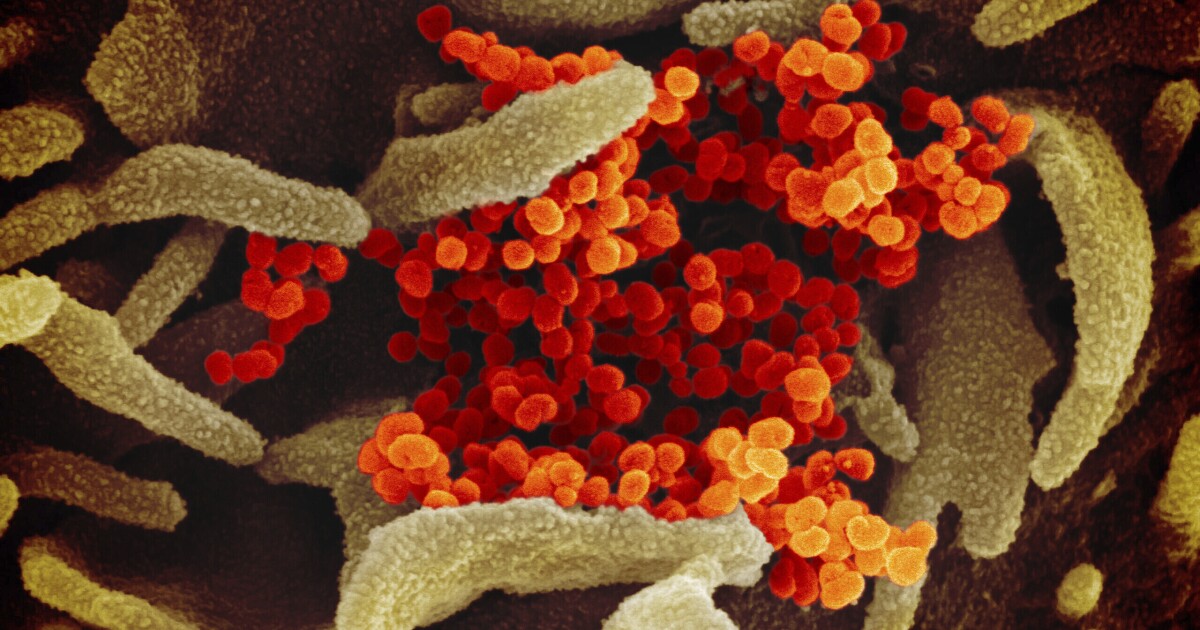
It is already known that SARS-CoV-2, the virus that causes COVID-19, can mutate to evade the vaccine against infection.
The Ómicron variants -BA.1, B1.1 and BA.2- can reinfect those who were previously infected by others, even when they are inoculated.
A third booster dose offers some protection against Omicron, but this wears off after three to four months, leaving most people susceptible to reinfection. Despite this, immunity transmitted by previous infection or vaccination continues to dramatically reduce the incidence of hospitalization and death.
We have also come to realize that our main saviors against COVID-19 are not antibodies, but another part of the immune system: T cells. Studies show that the strength of our long-lasting response to virus proteins -especially by those that recognize the spike protein- is strongly correlated with the degree of defense.
There are two types of T cells, CD4+ and CD8+, which are distinguished by the proteins on their surface. Since the former collaborate mainly in the production of antibodies, the latter are the true heroines of the story. Once they identify an invader they remember from a previous encounter, they move quickly to go in for the kill, demolishing infected cells and cutting off the life cycle of the virus.
Until Omicron, the differences in neutralization by vaccine-induced antibodies and by monoclonal antibodies were relatively minor.
But the process by which T cells recognize viral proteins is very different from that of antibodies, which record the structures of the intact viral protein.
We know that these critical structures, particularly those of the outer spike protein, differ from variant to variant. It is precisely this organized diversity that allows the virus to evade most of the antibodies made in response to natural infection and vaccination.
In contrast, T cells do not identify intact proteins. Rather, they record when a viral protein inside a cell is cut into short segments and cradled in the grip of a cellular protein called MHC type 1.
MHC type 1 presents the viral fragment to the T cell on the cell surface, where it can recognize the combination.
T cells examine and react to a wide range of viral protein fragments. In the case of SARS-CoV-2, they interact very little with regions of the virus that are sensitive to neutralization by antibodies. Therefore, T cell replication to viral infection is generally maintained in all variants.
With Omicron, vaccines using a viral protein elicited almost the same T-cell response to all strains. But now the situation has changed. Our type 1 MHC proteins are diverse, each identifying a unique set of viral protein fragments. Thus, our resistance to viral proteins depends on their sequence and that of our particular set of MHC type 1 proteins.
Consider a recent study by Gaurav D. Gaiha and colleagues, examining T-cell responses to Wuhan, Delta, and Omicron strains in people who have been infected, vaccinated and boosted, or infected and vaccinated, but not infected. reinforced. They found that most of those infected after inoculation respond with CD4+ and CD8+ strength and duration to all three variants.
But there was a worrying discovery. Approximately 20% of those inoculated showed a greater than 50% decrease in T-cell resistance to Omicron, compared to Wuhan and Delta. These poor responses were not correlated with sex or age, and follow-up experiments revealed that the difference was due to lower CD8+ reactivity, rather than CD4+ T-cell response.
The authors speculate that the inability of CD8+ T cells to defend against Omicron may be due to failure to identify the mutated peptides. Indeed, their theoretical calculations are consistent with the hypothesis that changes in the amino acid sequence of the Omicron spike protein underlie the observed blind spots in T-cell determination. Inherited differences in the ability to recognize specific fragments of the protein probably explain why some people cannot mount defenses against this variant. They also conjecture that “these individuals may have reduced protection against severe disease.”
One sobering conclusion is that Omicron has strayed so far from the original strain that 20% of the people in the study might not be fully protected from either infection or hospitalization and death. However, a third dose of the vaccine was found to increase the T-cell response 20-fold or more.
“Although the Omicron spike protein was able to escape from T cells in a subset of individuals,” Gaiha told me, “what we learned is that this deficiency in T cell recognition can be overcome by booster vaccination. Furthermore, we found that non-spike proteins could be attractive targets for second-generation antigens that protect against future SARS-CoV-2 evolution.”
Gaiha defends an optimistic interpretation, but Omicron warns that future variants may escape both antibodies and T-cell immunity. We cannot predict whether a strain will emerge that evades the ability of vaccines to protect against infection and disease. serious, but we must be prepared for that threat, lest we be left defenseless against it.
William A. Haseltine, scientist and entrepreneur, is president of ACCESS Health International, a global health think tank.
To read this note in English Click here
–