The role of the Nurse in Endobronchial Aspiration in Patient affected by Covid-19 and hospitalized in intensive care: risks and procedures.
A global war afflicts the world, a virus that has brought us to our knees, causing us to lose so many soldiers. COVID-19 is the main enemy. The war field the hospital, where many gendarmes are fighting this battle without equal.
Today we face a very common issue in intensive care and intensive care departments around the world: Endobronchial aspiration in positive Covid patients.
A very basic procedure in the operating units but which in this historical period turns out to be one of the most dangerous and risky for all health personnel due to the large dispersion of droplets.
What is Bronchoaspiration?
It is the procedure that allows us to remove secretions from the nasopharynx or trachea in patients unable to spontaneously expectorate.
When to aspirate a patient?
Endobronchial aspiration is not programmable, but is performed as needed.
The patient is aspirated when:
– On auscultation with a phonendoscope, hissing, gurgling and crackling sounds are perceptible (these sounds are sometimes detectable by placing a hand on the patient’s chest);
-The patient is toxic and becomes tachypnoic;
– Secretions are visible leaking from the tracheal stoma or orotracheal tube;
-Signs of respiratory distress: use of accessory muscles, jugular retraction, movement of the nasal fins;
-When the blood gas analysis shows a decrease in PO2 and an increase in PCO2.
How to perform the Bronchoaspiration maneuver?
There are two methods:
– Open Circuit Suction: in which the patient must be momentarily disconnected from ventilation;
– Closed Circuit Suction: in which the patient continues to be ventilated and there is no leakage of droplets.
Open circuit suction.

It is the most harmful to the patient and most dangerous to the operator. Stopping the ventilation accentuates
hypoxemia and causes him to lose PEEP (Positive end expiratory pressure).
Very often, however, we have found ourselves having to use this methodology to overcome the lack of closed circuits.
How to choose the suction catheter?
The inside diameter of the catheter should not exceed half the inside diameter of the cannula.
We need to double the size of the artificial air opening. For example, if I have a cannula diameter of 8mm I multiply it by 2 and I get that the 16 French catheter is the one that can be used in maximum safety.
How are secretions aspirated in a closed circuit?
– Position the patient in a semi-sitting position or at 30 ° if possible;
– Check the suction system: the suction pressure must be:
PREMATURE INFANTS: 40-80mm / Hg
CHILDREN: 60-100 mm / Hg;
ADULTI: 80-120 mm/Hg;
– Hyperoxygenate the patient through the ventilator for at least one minute;
-Choose the right catheter and open the tube package leaving it inside
– Connect the aspirator to the tube without contaminating it;
– Disinfect the insertion point of the bronchoaspiration tube on the Mount fitting with chlorhexidine spray;
– Wear the sterile glove in the dominant hand;
– Remove the tube with the sterile hand and wrap the tube in the hand until the tip is kept between thumb and forefinger;
– Puts the fan in STANDBY mode;
– Open the cap of the Mount fitting with the non-sterile hand;
– Insert the tube without aspirating until the appearance of the carinal reflex;
-Reactivate the ventilation;
– Retract the tube by 1-2 cm and activate the suction by occluding the valve;
– Begin to remove the tube with small rotational movements for a maximum of 10/15 cm;
-Before removing the tube, put the ventilator back in STANDBY mode;
– Remove the tube and close the cap of the Mount connection;
-Reactivate ventilation.
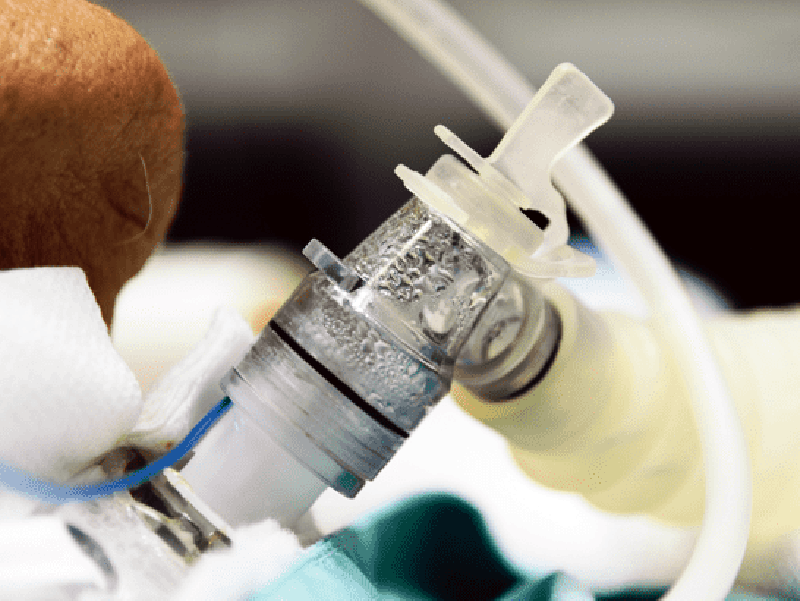
Closed circuit suction.
It is the safest system to use in patients with infectious respiratory diseases.

Is composed by:
-A fitting that allows connection to the endotracheal tube or to the tracheostomy tube;
-A swivel valve that allows the opening and closing of the circuit;
– A cap for washing the circuit;
-A suction catheter covered with a waterproof transparent protective sheath to be able to view the quantity and quality of the patient’s secretions;
The residence time of the circuit depends on the manufacturer’s indications. There are circuits on the market that can be used for a maximum of 24 hours and others, which represent most of the devices on the market, can remain in place for 72 hours.
–
:strip_icc():format(jpeg)/kly-media-production/medias/3084960/original/030467600_1585099572-virus-4915859_1920.jpg)
![[Preview 2020] Baltimore Ravens: the march to the top? | Touchdown Actu (NFL Actu) [Preview 2020] Baltimore Ravens: the march to the top? | Touchdown Actu (NFL Actu)](https://www.touchdownactu.com/wp-content/uploads/2020/08/Lamar_Jackson_preview_2020-1000x600.jpg)