05/25/2021 at 12:59 p.m. CEST
One of the key questions among researchers that could pose a new point in the coronavirus pandemic is how long does immunity last. The serological tests that many have used to find out if they had passed the disease only give us information about what is called innate immune response. That is, whether we have antibodies at that time or not.
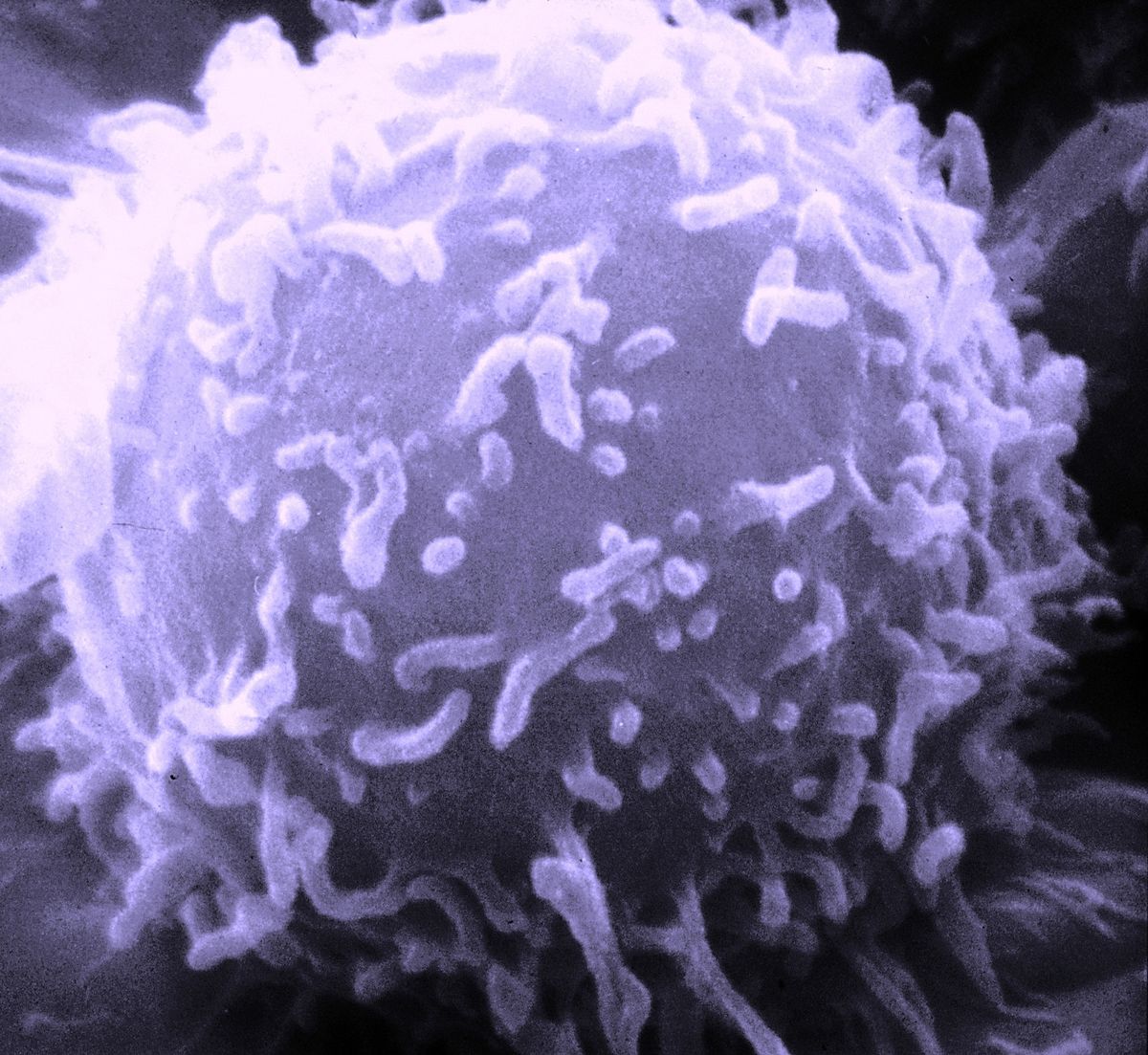
These antibodies come at a time when, once the infection is over, they go away. But there is another type of immunity, adaptive, conducted by Lymphocytes T, which develop from birth to around 25 years of age and are specific against each virus. It is an immunity that remains in our body and prevents further infections with these pathogens.
You may be interested in: “Killer T cells”: the great hope against new strains of the coronavirus
So know it cellular immune response during SARS-CoV-2 infection it is essential to know how the pandemic will continue to develop. Well, thanks to a study by the Infectious Disease Research Group of Vall d’Hebron Research Institute (VHIR) have been determined, for the first time for this virus, that the T lymphocytes with long-term resident memory remain in the lungs of people who have passed the infection which would fight against a possible reinfection.
In the acute phase of infection, researchers patterns identified in the response of T cells in the blood associated with the clinical course of patients.
Specific, hospitalized patients had higher levels of IFNg and IL-4 cytokines, while those with milder symptoms had more IL-10.
“IL-10 is a cytokine that may play an important role in controlling inflammation. If accompanied by an antiviral response, IL-10 creates an environment that promotes the resolution of the infection without promoting exaggerated inflammation, which is associated with the severity of COVID-19 ”, explains Dr Meritxell Genescà , Principal Investigator of the Infectious Diseases Research Group of VHIR.
More severe patients also have fewer T cells, since many of these cells die from overstimulation caused by the large inflammation generated by the infection. This death mainly occurs in the cells that produce IL-10, which makes the person’s condition worse.
The study was carried out with samples from 46 patients during the first wave of the pandemic: 14 people with symptoms not requiring hospitalization, 20 mild patients requiring hospitalization and 12 critically hospitalized patients.
Memory cells in the lung: a barrier to prevent re-infections
But not only has immunity been detected in the blood, but it has also been observed that the lymphocytes activated to fight viral infection have markers which indicate that they will travel from the blood to the lungs. For this reason, the persistence of resident T cells in the lung which would serve as memory cells to fight against possible future re-infections was analyzed.
This type of lymphocyte has been studied in seven recovering COVID-19 patients, who had had different clinical outcomes, taking advantage of the need to take biopsies for other causes in these people.
Have been found memory T cells in the lungs for up to 10 months after your infection, which would indicate that it would be a long-term memory. Thus, in the event of a new infection with SARS-CoV-2, the response against the virus would be localized in the lung.
“The respiratory tract is the entry route for the virus, therefore these cells would give a much faster and more efficient response, essential to limit its spread and disease,” adds Dr Genescà.
Resident memory T cells have already been described for other viral and bacterial infections in different organs and tissues. In the lungs, for example, some target cold or flu viruses, but this is the first time they have been identified for SARS-CoV-2.
Depending on the results, the Dr María José Buzón, Head of the Translational HIV Research Line in the Infectious Diseases Research Group of VHIR, comments that “to know if a person has an immune memory or not in case of infection, the analysis of antibodies or blood cells does not give us all the information, because the presence of T lymphocytes residing in memory in the lung is also important. “
Unfortunately, this is not possible in general medicine, as it requires a biopsy, a very invasive technique. In any case, it is relevant that these cells were found not only in people who transmitted the virus severely or very seriously, but also in those who showed only mild symptoms.
More knowledge for the generation of future vaccines
Among the results of the study, it also emerges that the type of immune response that develops in patients is related to the protein (s) that the immune system recognizes from the SRAS-CoV-2 when it enters the body.
This could open up possibilities for future coronavirus vaccines. Now all available vaccines target the SARS-CoV-2 S protein, a key protein for the virus to enter cells.
You may be interested in: How has the pandemic affected the health of our children?
But the new vaccines could include other parts of the virus, not just the S protein. The authors of the work point out that studying the types of immune response and which parts of the virus respond to the different memory profiles generated will help in the development of more effective vaccines.
To continue SARS-CoV-2 immunity investigationCurrently, VHIR researchers are conducting studies to analyze the differences between the immune response that occurs in naturally infected patients or in people who have been vaccinated.
The work, led by the VHIR Infectious Diseases group with Judith Grau and Nerea Sánchez as first authors, had the participation of the departments of infectious diseases, thoracic surgery, pathological anatomy and microbiology of the Vall University Hospital. of Hebron, of the Occupational Risk Prevention Unit and the VHIR Research Group in Diagnostic Immunology.
–