Oncology patients suffer from insomnia. When we talk about insomnia we refer to a difficulty falling asleep, staying asleep or having an early awakening. The complaint that most patients present is that sleep is not restful, because insomnia does not allow them to rest.
This problem can be transient, that is, of a short duration that is considered from 1 to 3 weeks. Or it may be a problem chronicwhen it extends beyond 3 weeks.
Epidemiology: some facts about insomnia
- In general, chronic insomnia affects 9-15% of the population.
- Between 1-2% of the population has primary insomnia, that is, for no reason.
- In Spain, 20% present at least one symptom of insomnia.
- It is stable through age.
- It generates a disability that lasts 3.5 days a month, which is very limiting.
- Increases the risk of alcohol consumption, falls, accidents. We must bear in mind that people who sleep poorly have daytime sleepiness during the day and drive, ride a motorcycle, ride a bike, climb stairs, etc.
Unlike other types of cancer, breast cancer is associated with higher levels of insomnia, with a prevalence between 38 and 61%. This means that, if we have 10 people with breast cancer, we can say that 4 to 6 people will have insomnia: a very high figure.
Pathophysiology: Why does insomnia occur?
In the general population, the aspects that influence insomnia are the following:
- Cognitive factors: bad beliefs or dysfunctional beliefs.
- Homeostatic dysregulators, such as naps.
- Alterations of circadian disruptors. The body works in a circadian rhythm: Each part of our body produces hormones at a certain time, some during rest, and this is repeated day after day. If we don’t rest, or we do it after hours, this cycle is altered.
- inhibitory factors. They are sleep hygiene problems that can be avoided if we change some habits.
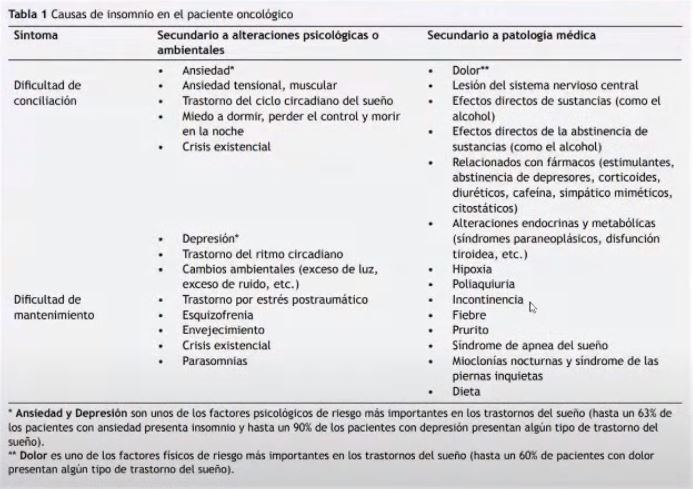
Causes of insomnia in cancer patients
- Secondary causes to psychological or environmental alterations.
The main cause that makes it difficult to fall asleep is anxiety. Other alterations are due to muscle tension, circadian rhythm disorders (night admissions to the hospital, with blood tests at night and rest during the day), fears, existential crises.
The causes that make it difficult to stay asleep are depression, again circadian rhythm disorders, environmental changes (excessive light or noise), post-traumatic stress, crises and parasomnias (people who talk at night, get up, or move uncontrollable with the feet).
- Causes secondary to medical pathologies.
The main cause of difficulty falling asleep is pain. The person who goes to sleep and is in pain obviously does not rest and does not sleep. Other causes for both falling asleep and staying asleep are lesions in the central nervous system, withdrawals, addictions to substances, drugs that stimulate (such as the corticosteroid that is tried to be given in the morning), diuretics (which increase the urinary rhythm) , thyroid problems, incontinence problems, polyachyria (increased urination frequency), hypoxia, fever, purito (itching), sleep apnea syndrome (snoring and shortness of breath), nocturnal myoclonus and restless legs syndrome, and some diet issue.
Diagnosis: how is insomnia detected?
Sleep can be treated by neurologists, psychiatrists, pulmonologists, psychologists, etc. In Primary Care, both the nurse and the doctor are the most important doors to the health system and see all kinds of patients. Many patients come to him with this pathology.
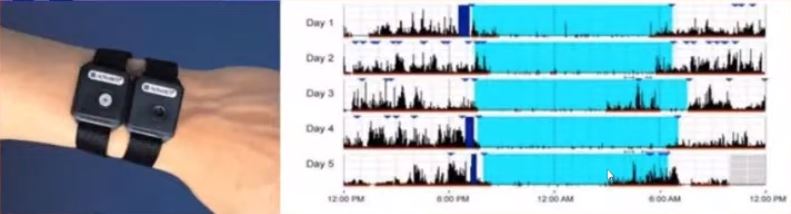
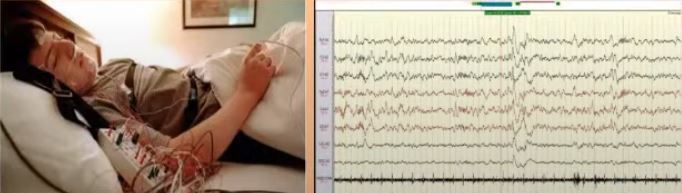
The doctor reviews the medical, psychiatric, psychological clinical history. Then he asks the patient what is happening to him and since when, and also asks him about his routines (naps), if it has happened before and medication, to detect if there is something that causes drowsiness or insomnia. The patient is then asked a sleep diary between 7 to 14 days. Poor sleep can be subjective and journaling can help establish a pattern. And, finally, an actigraphy and a polysomnography can be done.
Normally cancer patients express their complaints. It is normal for there to be episodes of insomnia. But there are so many concerns that many times not even the doctor asks about the patient’s insomnia and rest. On the other hand, when the doctor asks the patient what worries him, they rarely answer insomnia. However, if you don’t sleep, you don’t rest and you can’t be well during the day.
In addition, insomnia is a risk factor for worsening other cardiovascular problems, such as hypertension, myocardial infarction, or heart failure. It is also a risk factor for obesity and diabetes 2. Not sleeping well is like a little torture that can even lead to suicidal ideation. It is a problem that increases sick leave and traffic accidents. In short, it should be given much more relevance to sleeping well and resting.
Treatment: what to do to reverse insomnia?
To treat insomnia, pharmacological treatment is combined with cognitive behavioral therapy during the first month. Once the month passes, pharmacological treatment is not recommended, and only cognitive behavioral therapy should be used. But in practice, it is difficult to withdraw the medication and treatments are lengthened.
Pharmacological treatments:
- Benzodiazepines are the most common drug. In low doses they relax and in high doses they are hypnotic. One thing that works well is very difficult to leave. For this reason, it is customary to lower the dose and combine it with other relaxing activities.
- Sedatives are not used as much.
- There is very little evidence to recommend melatonin.
- Antipsychotics and antihistamines are not recommended at all.
What are cognitive behavioral treatments?
65% of patients respond to this treatment.
The cognitive teaches us to recognize and change the beliefs that make us unable to sleep well. It helps control negative thoughts and understand why worries keep us awake.
Behavioral helps us develop good habits at bedtime. There are many techniques and they can be individualized to each patient according to the needs of each person:
- Stimulus control therapy. It is a way to eliminate the factors that condition the resistance to falling asleep:
- Learn to have a consistent schedule for both getting up and going to bed. This is something basic that is not always done.
- Avoid naps, even short ones.
- Using the bed only for sleeping or for pleasurable sexual intercourse.
- Leave the room for 20 minutes if you can’t fall asleep.
- sleep restriction. This therapy is harder. It’s about staying awake all day if you haven’t slept at night, to get to the next night tired and sleep. This creates a constant habit. We cannot force the body to create the habit of being in bed and sleeping.
- Sleep hygiene. It consists of changing very basic habits.
- Do not smoke or drink two hours before going to sleep. The problem is that if you don’t drink for two hours, you might wake up thirsty. You can take a few sips before going to sleep. We can go through an excess and have to get up to urinate as well as a defect and we are thirsty.
- It is recommended to leave meals one hour before going to bed.
- Do not do intense exercise before sleeping.
- Do relaxation exercises.
- Improved sleeping environment.
- I couldn’t have a TV. With phones, tablets, televisions in the rooms, it makes us not disconnect. The blue spectrum slows melatonin secretion, creating a feeling of alertness and making it difficult to fall asleep. That is why it is essential to avoid it.
- Neither is a disco-type lamp.
- It can’t be a cold place.
- There should be no bright colors, but it should be a relaxed place.
- Avoid clocks.
- mindfulness sessions (relaxation training).
- There are apps created expressly to treat insomnia and the literature states that they are useful. Sleep is an example. Many of them are in English. It is recommended to use them before going to bed, because being in bed with the phone or tablet is counterproductive.
Conclusions
- Insomnia has unknown causes. We do not know why it occurs, but we can try to know the trigger.
- The diagnosis is usually made by talking with the patient and the clinical history.
- The treatment is not always pills. Cognitive behavioral therapy can be very helpful.
- The administration of sleeping pills can help for a short time, although it is advisable not to keep them for a long time.
References
Edinger et al. Clinical psychology review 25 (2005) 539-558
Insomnia in the cancer patient Nataly Contreras-Molinedos
 Valentí Aragunde-
Valentí Aragunde-
Family and community doctor. He is currently a tutor and teaching coordinator at CAP Casanova.
–
–