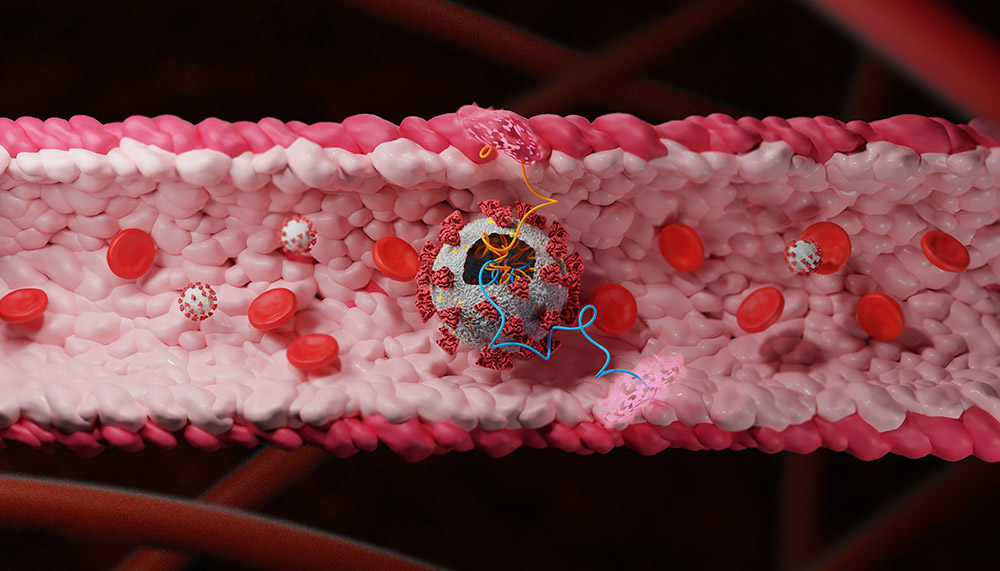
Three out of 29: Researchers have found out which proteins of the SARS-CoV-2 coronavirus attack our blood vessels. Accordingly, 18 of the 29 viral proteins contribute to disrupting the function of the vascular wall, but three non-structural proteins have the greatest impact – molecules that neither belong to the spike protein nor are involved in the rest of the viral envelope. These three proteins also promote the release of inflammatory messenger substances in the blood vessels and thus contribute to thrombosis.
Already relatively early in the course of the corona pandemic, it became clear that the coronavirus not only affects the respiratory tract and lungs, but also attacks the blood vessels and blood. Inflammatory changes in the vessel walls and lasting changes in the blood cells occur. As a result, many Covid-19 patients suffer from thromboses, embolisms and strokes and the blood flow to the lung tissue is impaired. The sometimes unnoticed shortness of breath in some patents could also be traced back to such circulatory disorders.
Manhunt for viral proteins
“Everything indicates that the coronavirus is seriously damaging the blood vessels or the endothelial cells that line them,” explains senior author Ben Maoz from Tel Aviv University. “Covid-19 is therefore not only a respiratory disease, but also a vascular disease.” However, it was previously unclear how exactly SARS-CoV-2 attacks the blood vessels and which of its viral proteins it uses for this.
To clarify this, Maoz, first author Rossana Rauti and her team have systematically examined which of the 29 proteins in the coronavirus are involved in damaging the blood vessels. To do this, they equipped harmless lentiviruses with a viral protein each and added them to cultures of human endothelial cells. They then used the conductivity to test, among other things, whether the vascular wall barrier formed by these cells was still intact and analyzed the cell metabolism of the affected cells.
Three out of 29 are particularly harmful
The result: the researchers found a vascular damaging effect for 18 of the 29 coronavirus proteins. But contrary to what one would expect, it was not the spike protein or other proteins involved in the envelope structure of SARS-CoV-2 that caused the greatest damage. Instead, Maoz and his team identified three non-structural proteins of the coronavirus as the most aggressive endothelial damage.
“These three viral proteins not only impair the integrity of the endothelial barrier, they also lead to increased release of the coagulation factor VWF and the release of cytokines,” the scientists report. These proteins thus actively contribute to the fact that the blood clumps and that there are inflammatory changes in the blood vessels. In the brain and lungs in particular, this contributes to the complications that are typical for severe courses of Covid-19.
Above all, non-structural proteins are harmful
It is also interesting to know which viral proteins are involved: two of these proteins, nsp-2 and nsp-5, are known to counteract the immune defense of the cells. They are only produced after the cell is infected and, among other things, block the release of antiviral messenger substances, as the team reports. The third protein, on the other hand, belongs to a complex that is part of the viral RNA polymerase – the enzyme that is crucial for the virus to multiply.
Using a model, the scientists also determined that two other non-structural proteins from SARS-CoV-2, nsp4 and nsp11, are also particularly damaging to other types of endothelial cells. In some cases, these viral biomolecules interacted with up to 40 proteins in their target cells and disrupted their function, as the tests showed.
Potential drug targets
According to Maoz and his team, these findings could help to better understand the vascular damaging effects of SARS-CoV-2 and to counteract them in a more targeted manner. So far there are only a few effective ways to treat severe courses of Covid-19 and the accompanying vascular damage.
“The data presented in our work give us a better insight into the mechanisms by which vessels and cellular systems are attacked by the virus,” explains Maoz. “By specifically targeting the proteins that are dominant for these effects, this enables us to develop active substances against the virus more quickly.” (ELife, 2021; doi: 10.7554 / eLife.69314)
Source: Tel-Aviv University
–