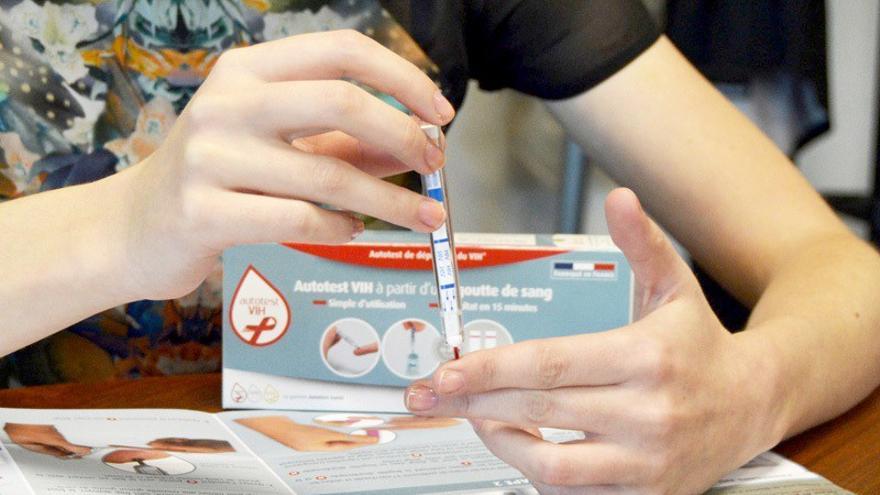
It is estimated that in our country there are between 160,000 and 170,000 infected with HIV, of which 14% are not diagnosed
According to UNAIDS estimates, between 160,000 and 170,000 people in Spain are living with the human immunodeficiency virus (HIV). And 14% are undiagnosed.
Currently patients have to take the antiretroviral treatment (a combination of medicines to suppress the replication of HIV), as your immune system is unable to control the virus on its own.
It is a disease for which there is no cure yet, but it has a very effective and safe treatment.
And now, an investigation opens up new hope.
Results from the biotech company AELIX’s HTI vaccine clinical trial results, in collaboration with Gilead Sciences, show that this injection can improve the response against the virus.
This new investigation, recently published in the scientific journal Nature Medicine, was conducted on 45 patients (44 men and 1 woman) with viral suppression for at least one year, which means that the amount of HIV in the blood is very low.
Our T-cell vaccine approach has the potential to play a pivotal role in strategies to treat HIV infection.
To study its effectiveness, once this was administered vaccine participants temporarily stop antiretroviral treatment, and virus levels in their blood are measured weekly for six months.
Therefore, we evaluated the efficacy of vaccination and how the use of AELIX HTI vaccine could allow patients to stop antiretroviral therapy (ART) for an extended period of at least six months.
As the Doctor Christian Branderco-founder and scientific director of AELIX:
- “Our T-cell vaccine approach has the potential to play a critical role in strategies to treat HIV infection.”

Of all the patients analyzed (15 received placebo and 26 vaccines), 41 discontinued treatment and were studied for a total of 24 weeks.
The result was:
- 40% of those who received the vaccine managed to go six months without this treatment.
- In the placebo group, all but one of the participants had to restart treatment before twelve weeks.
This vaccine “allows us to improve the suppression of the virus without drugs”
This is like the Dr. Beatrice Motheprincipal investigator of the Fight Against Infections Foundation study and research associate at the IrsiCaixa AIDS Research Institute.
- “The positive results of this study demonstrate that it is possible to induce an immune response in a person living with HIV, allowing for better suppression of the virus in the absence of antiretroviral drugs.”
The second phase of the clinical trial, which will begin in the coming months, called AELIX-003, aims to investigate the safety, tolerability and efficacy of the vaccine in combination with the Toll-Like 7 (TLR7) receptor agonist, in 57 people with HIV on antiretroviral therapy (ART).
Devi SenGuptadirector of the HIV cure development program at Gilead Sciences, points out that the path to a cure for this disease “is a complex scientific challenge and collaboration is the key to catalyzing research.”

HIV and AIDS, are they the same thing?
HIV is not the same as AIDS, as explained to this portal, on the occasion of World AIDS Day, the doctor Vicenç Falcóhead of the infectious disease service of the Vall d’Hebron hospital.
- “They are different stages of the same disease. And is that this virus affects the defenses and when they are very deteriorated the complications begin (opportunistic infections due to weakened immune system), which is what is known as like it (Acquired immunodeficiency syndrome)”.
That is, AIDS is the final stage of HIV.
What are the symptoms of HIV?
The symptomatology of the infection develops in three stages:
- The first stage goes unnoticed. It occurs between 2 and 4 weeks after infection and can cause symptoms very similar to those of the flu.
- In the second phase, called chronic, the retrovirus continues to infect cells, albeit very slowly. This is why medication with antiretroviral drugs is crucial. If the patient follows a proper treatment and undergoes regular checkups, the infection can become chronic, make it undetectable and never develop AIDS.
- In the third and final phase, the virus has multiplied dramatically and the patient’s immune defenses are unable to respond.
However, patients under treatment block the “natural history of the virus” so as not to develop AIDS and, therefore, other associated diseases such as:
- Pneumonia.
- Candidiasis.
- Tuberculosis.
- Cytomegalovirus.
- Cryptococcal meningitis.
- Toxoplasmosis.
“There is also a number of cancers associated with this immunosuppression, and it is worth highlighting the Kaposi’s sarcomaa skin cancer that causes patches of abnormal tissue under the skin or certain lymphomas (blood cancers)
How is HIV spread?
HIV is transmitted in four fluids: blood, semen, vaginal secretions and breast milk. This means that it can be transmitted through three routes: sexual (anal, vaginal or oral), blood and from mother to child.
- It is not transmitted by saliva, tears or sweat.
- Nor from insect bites
- And not even by contact with pets.
Undetectable = not transmissible
Currently, there are several drugs for people with HIV, which are increasingly “potent, better tolerated, almost free of toxicity and easy to take”.
Today the vast majority of patients have to take only one pill (a few years ago the treatment consisted of a cocktail of pills), which has improved the quality and Life expectation“which comes close to uninfected people”.
- But one of the best news is that antiretroviral treatment can “eliminate this virus to the point where it’s undetectable.”
This means that the viral load cannot be detected in blood tests, which causes “the disease to not progress and the immune system to recover”.
And another of the great advances has been ensuring that, if the viral load is undetectable, the disease is not transmitted “sexually, but through blood.”
How is HIV transmission prevented?
- Use a condom (both male and female) when having penetrative sex, whether oral, vaginal, or anal, with someone who is infected or whose infection is unknown.
- Know the risk of exposure from different sexual practices and the serological status of sexual partners.
- Avoid sharing syringes, needles, and other injection materials, such as skin-piercing tools for body piercing or tattooing.
- Regularly do blood tests to detect sexually transmitted diseases.