Foods high in saturated fat like red meat are already well documented as a major risk factor for colon cancer, as are a family history, inflammatory bowel disease (IBD), smoking and diabetes. type 2. It is believed that diet strongly influences the risk of colorectal cancer, and that changes in eating habits could reduce the risk of this cancer by up to 70% (Source CDC). Finally, of all colon cancer risk factors, diet is the most easily controlled lifestyle factor.
–
Strong link between obesity and increased risk of tumor
Building on this already known link between obesity and increased risk of colorectal cancer, Arizona State Dr. Miyeko Mana’s team focused on bowel stem cells, most likely the cause. of cancer and has been able to decipher the entire molecular cascade initiated by a high-fat diet and leading to bowel and colon cancer.
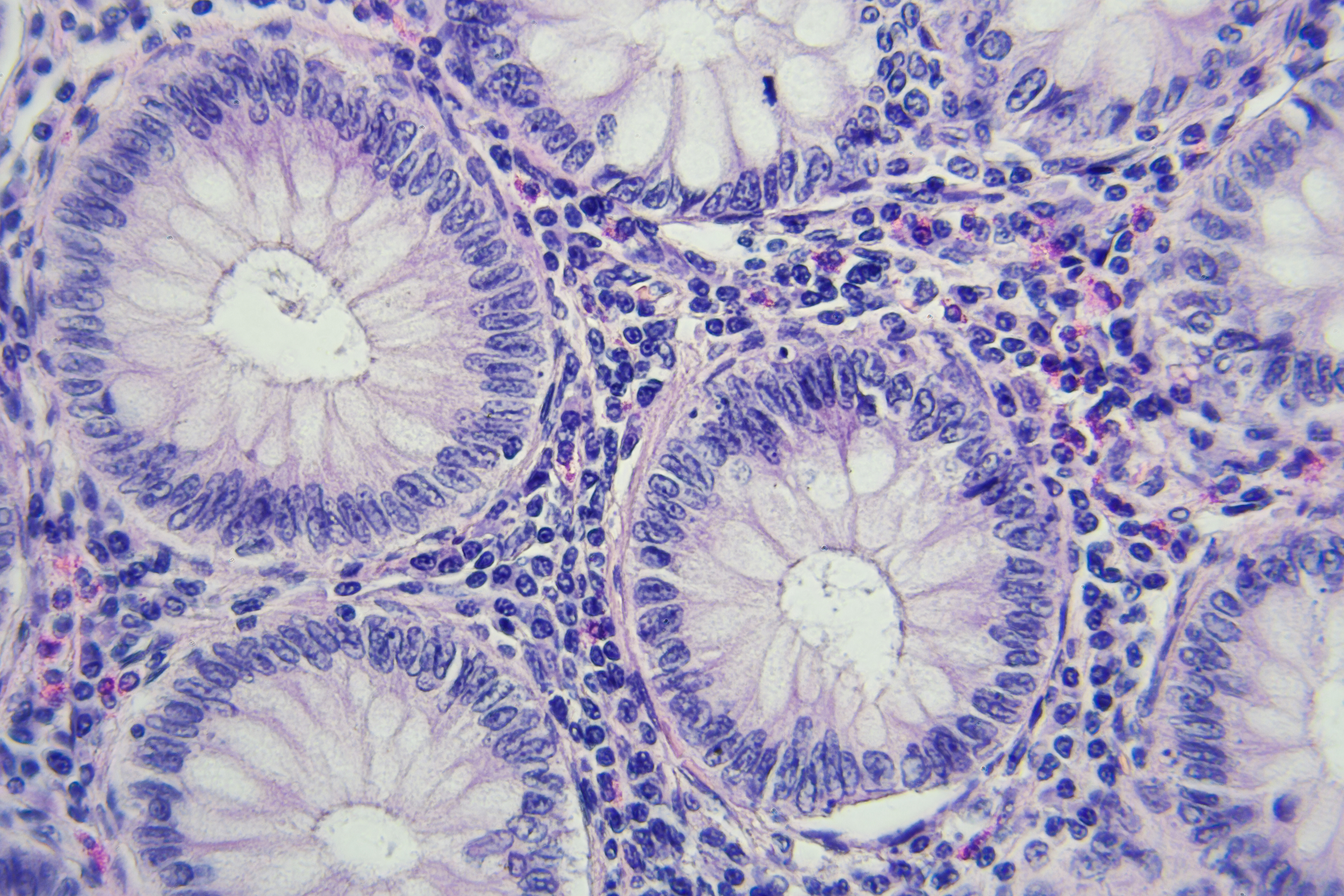
Stem cells vs high fat diet: As food is broken down and passes through the intestine, it interacts with intestinal stem cells (ISCs) found all along the inner surfaces of the intestine. These ISCs grouped together in crypts contain fat-sensing molecules that detect and respond to fat in food. Researchers have studied the mechanisms necessary for stem cells to adapt to a diet high in fat.
Cancer-triggering receptor proteins: at the center of this mechanism of adaptation of stem cells to high fat diets are receptors activated by ” peroxisome proliferators ”or PPAR (peroxisome proliferator-activated receptor). And some PPARs trigger a cellular program that increases the risk of cancer. There are several families of PPAR, scientists have sought to better define their respective roles in mice fed a diet high in fat. The activity of each PPAR has been carefully monitored to understand its effects on cancer risk.
2 PPAR delta and PPAR alpha receptors play a key role in the risk of colorectal cancer associated with a high fat diet. By molecular sequencing of cells from different areas of the small intestine and colon, the researchers show that the 2 PPAR proteins target a mitochondrial protein, Cpt1a, necessary for the import of long chain fatty acids (LCFA) into the mitochondria . A mouse deprived of the Cpt1a gene and fed a rich diet no longer develops a tumor: the loss of Cpt1a blocks the uncontrolled proliferation of ISCs in the crypts.
- The deletion of a protein, Cpt1a, protects against this high fat diet phenotype in intestinal stem cells, and thus reduces the risk of colorectal cancer.
If this work confirms that the levels of fat in the diet have a direct impact on intestinal stem cells, and decipher the underlying process, they also suggest that targeting these 2 proteins PPAR and / or CPT1a could protect the intestine from cancer. development of tumors.
It is now time to use these results to better treat human colon cancer. “Because all the studies to date have been carried out on model mice…”.
–