【Health and Welfare News】 It was confirmed that Yonsei University Health System (Director Geum Ki-chang) had treated 355 prostate cancer patients as of November after opening the fixed treatment room at the Jungian Treatment Center in April last year.
Additionally, since the opening of the gantry treatment room last May, it has been reported that a total of 57 patients, including 45 with pancreatobiliary cancer, 6 with liver cancer, and 8 with lung cancer, have been treated.
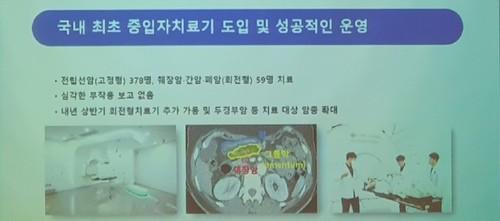
According to data from the Intermediate Therapy Center released by Yonsei Medical Center on the 19th, 378 people with prostate cancer were treated in the fixed treatment room, and 59 people with lung cancer, liver cancer, biliary tract cancer, and pancreatic cancer were treated in the gantry treatment room.
It was confirmed that the cost of treatment for prostate cancer was 50 million won, with a treatment profit of about 18.9 billion won, while the average treatment cost for lung cancer, liver cancer, biliary tract cancer, and pancreatic cancer was 80 million won, with a treatment profit of 4.5 billion won.
The average waiting period for intermediate treatment at Yonsei Medical Center is 4 to 6 months. Accordingly, Yonsei Medical Center is preparing to open a gantry treatment room in the first half of 2025. After the first half of 2025, when all three treatment rooms are operational, the treatment area will expand to include solid cancers such as head and neck cancer and osteosarcoma, and it is expected that approximately 1,200 cancer patients will be able to receive heavy ion treatment per year.
Meanwhile, the heavy ion therapy device installed at Yonsei Medical Center is the 16th heavy ion facility in the world, and operates three treatment rooms (one fixed treatment room and two rotational treatment rooms).
‘Heavy ion treatment’ targets cancer cells more precisely than existing radiation treatments, has fewer side effects and is more effective, so it is called ‘dream cancer treatment’ at the Heavy Ion Treatment Hospital.
Heavy ion therapy is a radiation treatment using carbon particles that has recently been attracting attention, and has a much more powerful destructive power than existing X-rays or gamma rays. This treatment is carried out by using an accelerator to raise carbon particles to a speed close to the speed of light and then directly hitting the cancer cells to destroy them.
The 5-year survival rate for pancreatic cancer is only 10%. However, according to the Japan Institute of Radiology (QST), for patients with pancreatic cancer whose stage is advanced and surgery is not possible, when anticancer drugs and baryon therapy were combined, the two-year local control rate improved to 80%. The local control rate is the probability that cancer will not recur in the treated area and is a key indicator of treatment performance in heavy ion therapy targeting a specific area. The two-year survival rate after heavy ion treatment was reported to be 56%, proving excellent treatment effectiveness.
Radiotherapy for liver cancer is difficult. Due to a small number of nerve cells, pain cannot be felt easily, so the diagnosis is delayed and the disease is initially diagnosed at an advanced stage. In addition, liver function is reduced due to cirrhosis, so there is a high risk of hepatotoxicity due to radiation. Heavy ion therapy has the characteristic of focusing high-dose radiation only on cancer cells and avoiding normal cells, which can reduce side effects while increasing treatment effectiveness.
The two-year local control rate for liver cancer patients who received baryon treatment at Gunma University Hospital in Japan reached 92.3%. QST’s clinical study recorded a 5-year local control rate of 81%. In particular, even when the tumor size was larger than 4 cm, the 2-year local control rate was 86.7% and the 2-year survival rate was high at 68.3%.
If necessary, heavy ion therapy can be used in conjunction with existing treatments such as chemotherapy to increase treatment effectiveness. In particular, in cases such as pancreatic cancer or liver cancer, which are diagnosed late in the diagnosis at an advanced stage and surgery is difficult, depending on the patient’s condition, the size of the cancer is reduced with chemotherapy, etc., and then the intermediate treatment is continued.
Director Geum Ki-chang of the Medical Center said, “There have been no reports of serious side effects so far, and patient satisfaction is very high. If we operate additional rotary treatment devices in the first half of next year, the scope of application will expand to include head and neck cancer, and the number of patients treated will increase.”