A study has found that removal of the thymus gland increases the risk of death and cancer.
Although it is involved in the development of immune function, it gradually degenerates with the maturation of the human body, and unlike in adults, where it was considered safe to remove it because its function was unclear, thymectomy in adults resulted in a worsening prognosis.
The results of a study on the correlation between thymus removal and health in adults, in which Professor Cameron A. Kooshesh of the Center for Regenerative Medicine at Massachusetts General Hospital in the U.S. participated, was published in the international journal NEJM on the 3rd (DOI: 10.1056/NEJ Moa2302892).
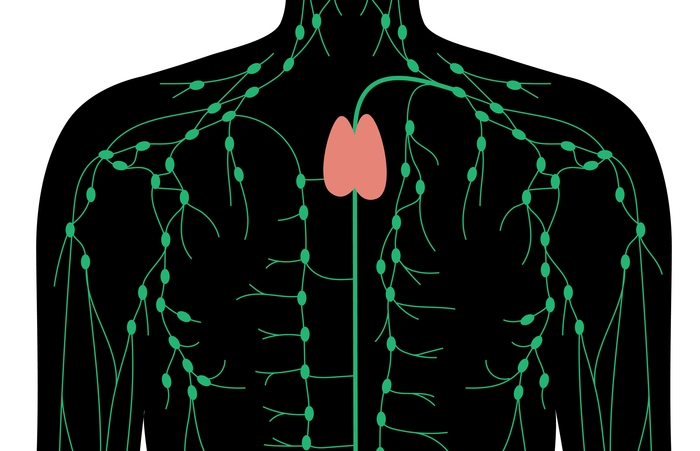
Located behind the breastbone and in front of the heart and aorta, the thymus gland is an organ that makes immune cells. It started to develop in newborns, reached its largest size during puberty, then degenerated, and changed to small adipose tissue in adults, after which its function was thought to be unclear.
A study has found that removing the degenerated thymus gland after adulthood increases the risk of cancer and death.
In particular, as it is known that thymectomy is effective in the treatment of myasthenia gravis, thymus removal is being performed in various surgical procedures including myasthenia gravis.
The researchers hypothesized that even in adults, the thymus gland is required to maintain immunity and overall health, and in a cohort comparing mortality, cancer and autoimmune disease rates in adult patients who underwent thymectomy with a control group who underwent similar thoracic surgery without thymectomy. embarked on
Registry-enrolled 1420 patients who underwent thymectomy and 6021 controls were included in the study, and 1146 of the patients who underwent thymectomy had a demographically matched control group.
As a result of the analysis, the all-cause mortality rate at 5 years after surgery was 8.1% in the resection group and 2.8% in the control group.
There was no significant difference in the risk of autoimmune disease among the groups in the entire cohort, but when patients with preoperative infection, cancer, or autoimmune disease were excluded from the analysis, the autoimmune disease rate was higher in the resection group at 12.3% versus 7.9%.
The results were similar when the follow-up period was extended to more than 5 years.
All-cause mortality was higher in the thymectomy group than in the general population (9.0% vs. 5.2%), and mortality from cancer was higher (2.3% vs. 1.5%).
A subgroup of patients (22 thymectomy patients, 19 control patients) for whom T cell production and plasma cytokine levels were measured was followed up for an average of 14.2 years after surgery. wrote
This means that the thymus is mostly replaced by fat in adulthood and degenerates, but it is still in charge of ‘functions’ such as generating T cells.
“This study confirmed that all-cause mortality and cancer risk were higher in patients who underwent thymectomy,” said the researchers. When excluded from the analysis, it was found to be associated with an increased risk of autoimmune disease.”
2023-08-03 02:53:16
#thymus #useless #organ.. #Increased #risk #death #cancer #resection