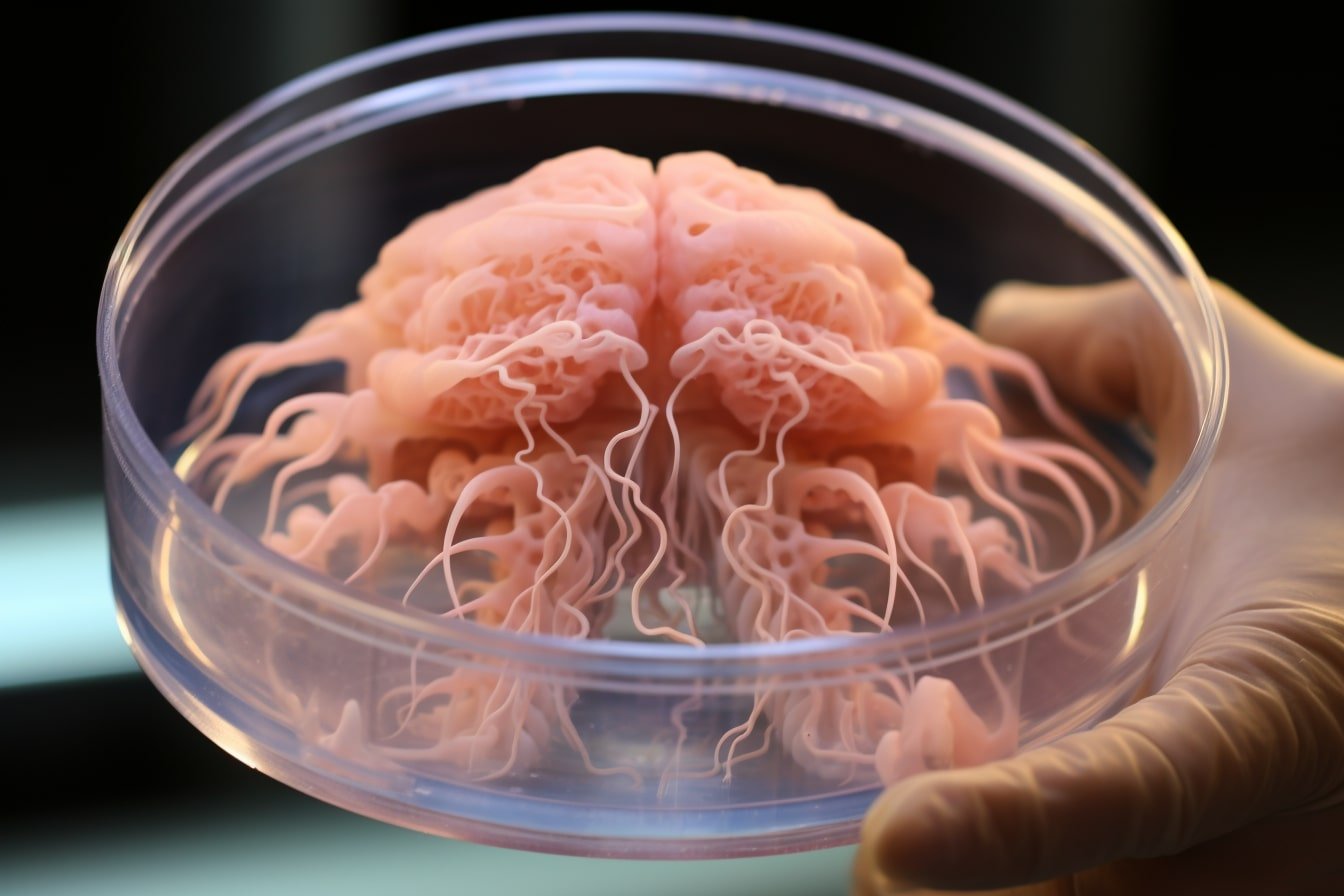
Researchers at the University of Michigan have developed a method to produce lab-grown mini brains, known as human brain organoids, free of animal cells. This breakthrough could lead to more accurate studies and treatments for neurodegenerative conditions such as ALS and Alzheimer’s.
Previously, brain organoids were grown using a substance derived from mouse sarcomas called Matrigel, which led to inconsistencies due to its undefined composition and variability. The new method uses an engineered extracellular matrix without animal components, improving the neurogenesis of brain organoids.
The use of human brain organoids as an alternative to mouse models has been explored over the last decade in the study of neurologic diseases. These 3D tissues derived from stem cells more closely resemble the complex structure of the human brain compared to conventional two-dimensional cultures.
The new method developed by the University of Michigan uses an engineered extracellular matrix free of animal components, overcoming the previous method’s variability issues. The researchers found that the lab-grown organoids using this new method showed enhanced neurogenesis compared to previous studies.
This breakthrough allows for more accurate replication of human brain conditions and opens doors for personalized treatment of neurodegenerative diseases. The method allows for potential reprogramming with cells from patients suffering from these diseases, paving the way for personalized treatments.
The success of these xenogeneic-free human brain organoids also opens the door for reprogramming with cells from patients with neurodegenerative diseases. This could allow researchers to build mini brains that mimic the conditions of individual patients, helping to investigate possible treatments and model disease progression on a personalized level.
The researchers at the University of Michigan used an engineered extracellular matrix comprised of human fibronectin, a protein that serves as a native structure for stem cells to adhere, differentiate, and mature. The organoids were cultured for months, even during the COVID-19 pandemic when lab staff were unable to enter the building.
Using proteomics, the researchers found that their brain organoids developed cerebral spinal fluid that closely matched human adult CSF compared to previous studies using Matrigel.
This advancement in the development of human brain organoids free of animal components will significantly improve the understanding of neurodevelopmental biology and make it easier for translational research to make its way from the lab to the clinic, according to senior author Joerg Lahann, director of the U-M Biointerfaces Institute.
The researchers believe that this breakthrough could revolutionize the study and treatment of neurodegenerative diseases by providing more accurate models and personalized approaches.

What were the limitations of previous methods that used Matrigel in the development of brain organoids?
The limitations of previous methods that used Matrigel. The researchers combined human stem cells with a customized hydrogel to create a scaffold that supports the growth and differentiation of brain organoids.
The engineered extracellular matrix provides a more defined and consistent environment for the development of brain organoids. This allows for better control and reproducibility in experiments, leading to more accurate and reliable results. By eliminating animal components, the new method also addresses ethical concerns and reduces the risk of contamination by animal-derived pathogens.
One of the key advantages of using human brain organoids is their ability to mimic the complexity of the human brain. These mini brains contain different cell types and exhibit similar patterns of gene expression and neural circuitry as the human brain. This makes them a valuable tool for studying neurodegenerative conditions such as ALS and Alzheimer’s, which are difficult to replicate in animal models.
With this new method, researchers can now study the development and progression of neurodegenerative diseases in a more accurate and realistic model. They can observe how specific genes and environmental factors contribute to disease onset and progression, and test potential treatments in a human-like environment.
In addition to their applications in research, human brain organoids could also be used for personalized medicine. By using a patient’s own cells to create organoids, researchers can study the individual’s disease progression and response to different treatments. This could lead to more targeted and effective therapies for neurodegenerative conditions, improving patient outcomes.
Overall, the development of animal-free human brain organoids is a significant breakthrough in neuroscience research. It provides a more accurate and reliable model for studying neurodegenerative diseases and paves the way for better treatments and interventions.


This innovative method of producing lab-grown mini brains without the use of animals is a significant step forward in neurodegenerative disease research. It not only provides a more ethical approach but also offers greater accuracy and reliability in studying these complex conditions. Exciting times for scientific advancements in the field!
This new method of producing animal-free lab-grown mini brains is a groundbreaking development for neurodegenerative disease research. It offers tremendous potential to help us better understand and find potential treatments for these complex conditions, while also promoting ethical research practices. Exciting times ahead for the field of neuroscience!