Researchers from the University of Cologne, Amsterdam UMC and the University of Copenhagen have discovered that targeted combination therapy without chemotherapy is more effective and has fewer side effects for patients with chronic lymphocytic leukemia (CLL). The results of their research have been published in the New England Journal of Medicine.
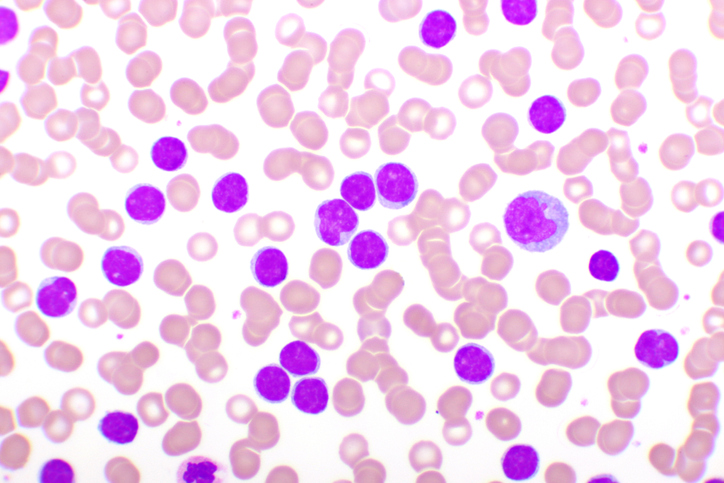
Chemotherapy is to date the most effective first-line treatment for relatively young patients with chronic lymphocytic leukemia (CLL). The disease is the most common form of blood cancer in the Western world and causes a significant health burden for patients and society.
Valuable information
Arnon Kater, professor of hematology at Amsterdam UMC and chair of the HOVON CLL study group, has been studying the behavior of CLL cancer cells in the lymph nodes and blood together with colleagues and collaborators for more than fifteen years, discovering valuable information about how cancer cells develop drug resistance and evade the immune system.
“CLL cells circulate in the blood and accumulate in the lymph node, where they can manipulate different cells in that microenvironment to promote their growth and survival,” explains Prof. Kater. “About five years ago, we saw evidence in preclinical studies that venetoclax and ibrutinib were a particularly effective combination. What happens is that ibrutinib banishes malignant cells from the lymph nodes into the bloodstream, where they are most vulnerable. Venetoclax then cleans them up.”
Traditional chemotherapy drugs work by killing rapidly dividing cells, including cancer cells, as well as normal healthy cells. However, venetoclax, ibrutinib and the antibodies used in this study are targeted therapies that specifically target the proteins and pathways that are overexpressed or dysregulated in CLL cells, leading to the selective killing of cancer cells while sparing normal healthy cells.
GAIA/CLL13
The phase 3 randomized GAIA/CLL13 trial was conducted in a total of 926 patients with CLL in 159 hospitals in 9 European countries and Israel. About a quarter of the patients came from the Netherlands. The patients were divided into four groups and received either chemotherapy and an anti-CD20 antibody (standard of care), or venetoclax in combination with an anti-CD20 antibody (either rituximab or obinutuzumab). The fourth group received a triple combination of ventoclax, obinutuzumab and the BTK inhibitor ibrutinib.
Results
At Month 15, the percentage of patients with undetectable minimal residual disease was significantly higher in the venetoclax-obinutuzumab group (86.5%) and the venetoclax-obinutuzumab-ibrutinib group (92.2%) than in the chemoimmunotherapy group (52.0%). %), but not significantly higher in the venetoclax-rituximab group (57.0%). The three-year progression-free survival was 90.5% in the venetoclax-obinutuzumab-ibrutinib group and 87.7% in the venetoclax-obinutuzumab group, compared to 75.5% in the chemoimmunotherapy group. Like detectable disease, progression-free survival was also not significantly higher in the venetoclax-rituximab group (80.8%).
“The data from this study confirm that the venetoclax-obinutuzumab combination is more beneficial than standard chemo-immunotherapy regimens,” says Prof. Kater. “In fact, the percentages of patients in the venetoclax-obinutuzumab and venetoclax-obinutuzumab-ibrutinib groups with undetectable minimal residual peripheral blood disease are among the highest reported in first-line therapy for CLL, at 86.5% and 92.2%, respectively . Regarding the data from the venetoclax-obinutuzumab-ibrutinib group in the current trial, we confirmed the phase 2 trial results showing promising progression-free survival. But whether the triple combination is even more beneficial than other targeted regimens needs more study.”
Mutated IGHV gene
The researchers also evaluated the efficacy of the treatment regimens with respect to the mutational status of IGHV, the variable region immunoglobulin heavy chain gene, which plays an important role in the immune system’s ability to recognize and respond to foreign substances. In CLL, the IGHV gene may or may not be mutated.
Unmutated IGHV in CLL means that the gene’s DNA sequence is the same as the germline version of the gene, with little or no changes. This is often associated with a more aggressive disease because the cancer cells are more similar to immature B cells and have a stronger ability to survive and proliferate. About 50% of CLL patients have non-mutated IGHV.
The researchers found that the percentages of patients with unmutated IGHV who had progression-free survival at 3 years were 65.5% (chemoimmunotherapy), 76.4% (venetoclax-rituximab), 82.9% (venetoclax-obinutuzumab), and 86. 6% (venetoclax-obinutuzumab-ibrutinib), but the percentages of patients with mutant IGHV who had progression-free survival at 3 years were not significantly different, 89.9%, 87.0%, 93.6%, and 96.0%, respectively.
“In our study, venetoclax-obinutuzumab or venetoclax-obinutuzumab-ibrutinib therapy provided a significant progression-free survival benefit in patients with non-mutated IGHV,” says Prof. Kater. “However, chemoimmunotherapy may still be better for patients with mutated IGHV at this point.”
Shorter treatment times
“With more drugs at our disposal, we can devise combinations that achieve better disease-free progressions, while at the same time reducing the risk of developing resistance to therapies through shorter treatment times,” says Prof. Kater. “By stopping certain periods of time and giving the drugs only when they are needed, you can reduce side effects, use the drugs for much longer and lower healthcare costs.”
Reference
2023-05-17 15:10:00
#Patients #CLL #benefit #targeted #combination #therapy #chemotherapy #NTVH