A review of the fungus outbreak in 2020 concluded that there were approximately 4,750 cases globally between 2009 and 2019.
The drug-resistant fungus Candida auris was only discovered about 15 years ago but is already one of the most dangerous hospital microbes in the world.
If it enters the body, this type of fungus can affect the bloodstream, nervous system and many internal organs, and the World Health Organization estimates that the death rate ranges from 30 to 53% of patients infected with the fungus.
Most worryingly, the fungus has been shown to be resistant to the most common types of antifungal drugs, and the BBC’s health correspondent James Gallagher says some strains are resistant to all known drugs.
According to the US Centers for Disease Control and Prevention, the fungal infection has spread to more than 30 countries, and a review of the spread of the fungus in 2020 concluded that there were nearly 4,750 cases globally between 2009 and 2019.
In a March 20 statement, the CDC said new data showed that the fungus “spread at an alarming rate in US healthcare facilities” in 2020 and 2021.
Clinical cases in the country tripled, from 476 in 2019 to 1,471 in 2021.
A 2019 study by an international team of researchers indicated that rising temperatures associated with climate change may have played a role in the rise in the number of Candida auris infections.
Here’s what you need to know about this deadly super mushroom:
What is Candida auris?
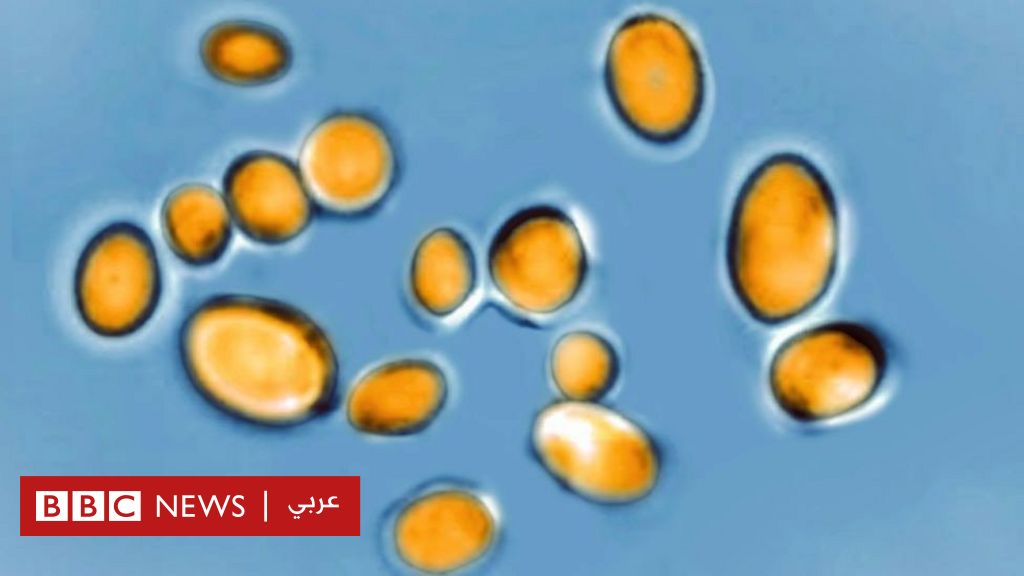
Candida auris is a genus of yeast, a family of fungi that contains species that are very useful to humans for activities such as bread making and beer brewing, but there are also species that cause infections in humans.
One example is the very common fungus Candida albicans, which causes thrush but can also lead to more severe infections
Candida auris was first discovered in the ear canal of a patient at the Tokyo Metropolitan Geriatric Hospital in 2009, which led to the fungus being named after it, as the word auris is Latin for ear.
Most of the time, the fungus lives on our skin without causing problems, but it can cause infections if we are not healthy or if it gets to the wrong place, like our bloodstream or lungs.
What kind of disease does it cause?
Candida auris often causes bloodstream infections, but it can also affect the respiratory system, central nervous system, and internal organs, as well as the skin.
These infections are usually very serious.
“The biggest problem with these fungi is their resistance to the drugs we have,” said Dr. Tina Joshi, assistant professor of molecular biology at the University of Plymouth in the UK.
“But another problem is that recognizing Candida auris infection is very difficult and can easily be confused with other fungi, which can lead to the wrong treatment.”
The wrong treatment means that the patient may be ill for a longer period of time, or get worse before the proper treatment is reached
How does it spread?
Transmission is mainly through contaminated surfaces in hospitals, sticking to intravenous tubes and blood pressure measuring devices, and Dr. Neil Stone, a fungicide expert at the Hospital for Tropical Diseases in Kings College London, says that cleaning surfaces is very difficult.
The solution is often to close entire wards.
“It’s the most worrisome fungus that we ignore despite the dangers it poses,” Dr. Stone said.
“It could shut down entire healthcare systems,” he added.
Should I be worried about getting an infection?
It is very unlikely that you will catch a Candida auris infection in your daily life.
The risk is higher if you stay in the hospital for a long time or if you’re in a nursing home, and patients in intensive care are more likely to develop a Candida auris infection, according to the CDC.
The risk of infection is higher if you take antibiotics often, because the drugs also destroy the good bacteria that can prevent entry of Candida auris
Why is Candida auris resistant to the usual medications?
Resistance to common antifungal drugs, such as fluconazole, has been observed in the majority of Candida auris strains.
This means that these drugs do not work for Candida auris. For this reason, less common antifungal drugs have been used to treat infections, but Candida auris has now developed resistance to these drugs as well.
And DNA evidence shows that antifungal resistance genes in Candida auris are very similar to those in the very common Candida albans.
This indicates that resistance genes may have been passed from one species to another.
How could climate change be responsible for the high numbers of infections?
A 2019 study published in the journal mBio of the American Society for Microbiology indicated that the reason behind the spread of Candida infections may be because these species are forced to live in higher temperatures due to climate change.
Most fungi prefer the cooler temperatures found in the soil. But as global temperatures rise, Candia auris has had to adapt to higher temperatures.
Fungi are often resistant to usual medications, making the infection difficult to treat
This may have made it easier for fungi to thrive in the human body, which is warm at 36°C to 37°C.
What can be done to control the number of infections?
Better understanding who is most susceptible to infection with Candida auris is the first step towards reducing the number of infections.
“We are behind in terms of studying fungi,” said Dr. Joshi.
“I’m not surprised at all, we’re now forced to catch up,” he added.
And health care professionals need to know that people who spend extended periods of time in hospitals or nursing homes or those with weakened immune systems are at greater risk.
Not all hospitals identify Candida auris in the same way. Sometimes they are confused with other fungal infections, such as thrush, and given the wrong treatment.
In a March 20 statement, the CDC said new data showed the fungus was “spreading at an alarming rate” in the United States.
Improving diagnosis will help identify patients infected with H. pylori early, which means giving appropriate treatment, and preventing the spread of infection to other patients.
But above all, infection prevention efforts must be improved, Dr. Joshi said.
“The main measure is infection prevention and control, because we have already seen how difficult it is to treat what is happening to patients,” he added.
“Hospitals must be at the forefront of disinfection and cleaning,” he said.