If on the territory the number of general medicine consultations per year and per inhabitant is less than 2.5; if the time between the first pharmacy in the town is more than 10 minutes away by road and access to emergency medicine (fire-fighters, on-call doctor, emergency doctor, etc.) is more than 30 minutes of transport, then it’s a medical desert.
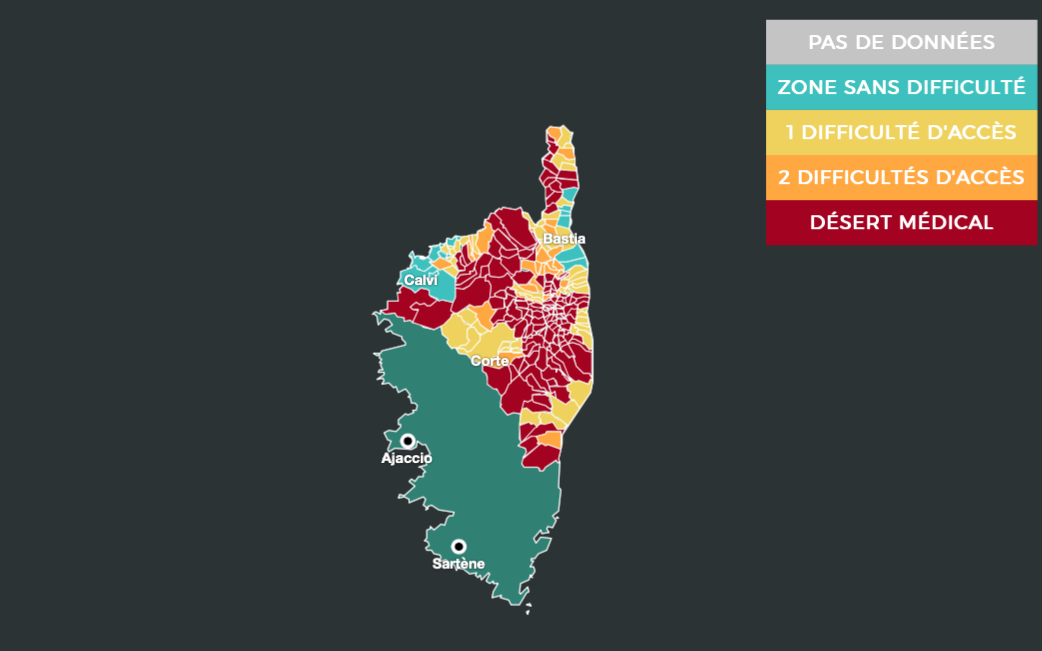
Great inequalities within the island
In Corsica, only 22 municipalities are considered as medical areas with good access to healthcare. They are mainly located in or near large cities. In Ajaccio for example, the study lists 4.4 consultations in general medicine per year and per inhabitant. There are also 31 pharmacies, 73 general practitioners and emergency care facilities throughout the city. Bastia is also spared with 4.5 consultations in general medicine, 26 pharmacies and 59 general practitioners.
On the contrary, in a rural municipality like Ventiseri which hosts 2,048 inhabitants a year, the situation is alarming. There are 1.5 consultations in general medicine per year and inhabitant. The nearest emergency treatment facility is a 65-minute drive away. The town has only one general practitioner and one pharmacy.
Marie Beaurenaud, spokesperson for Guide Santé explains her strong disparities: “Corsica is a very mountainous region where care is more distant but the limitation of access to care is also the result of the diagonal of the vacuum, there is a whole part of France where there is no one left . “
But how to overcome these strong inequalities?
Several solutions have been put on the table to fight against medical desertification. The development of telemedicine in these areas could be a viable means. However, this practice requires a good internet connection. However, very often, medical deserts correspond to the same territories as digital deserts. In Corsica in particular, access to a good connection is often very difficult to find. In addition, it is not possible to treat all pathologies by video.
To make up for the lack of doctors, Professor Guy Vallancien, member of the National Academy of Medicine, mentions the possibility of using advanced practice nurses (IPA) or front-line nurses. They would first go to the patient’s home to see if it is possible for them to find a solution on their own. If not, they would send the patient to a doctor or to the emergency room.
Marie Beaurenaud also mentions other alternatives such as multidisciplinary health homes, better cooperation between public and private structures as well as the establishment of itinerant health buses, which would be like a “tragulinu” of health.
To find the interactive map and see if your town is a medical desert click here.
– .